AHA19 Scientific Sessions came to an end last month and we all went back to our homes, but the discussions continued, especially concerning the ISCHEMIA Trial. The study design was very simple (Figure 1). This is a randomized parallel study of patients with stable coronary artery disease and moderate to severe ischemia. Ischemia was defined as ≥10% ischemia on nuclear imaging; ≥3 segments of ischemia by echography; ≥12% ischemia and/or ≥3 segments with ischemia by cardiac magnetic resonance; and ≥1.5 mm ST depression in ≥2 leads or ≥2 mm ST depression in single lead at <7 METs with angina on exercise treadmill testing. Initially, critical anatomy was ruled out by a Coronary Computed Tomography (CCT) ie Left Main disease ≥50%. Then patients were randomized to a routine invasive strategy on top of medical therapy (n = 2,588) versus medical therapy alone (n = 2,591). In the invasive therapy arm, revascularization was either surgical or percutaneous. In the medical therapy arm, angiography was performed if medical therapy failed. Coronary revascularization was performed in 80% of the invasive arm and 23% of the medical therapy arm. A total of 5179 patients were enrolled and followed up for a duration of 3.3 years. The primary endpoint (cardiovascular (CV) death, myocardial infarction (MI), resuscitated cardiac arrest, or hospitalization for unstable angina or heart failure) occurred in 13.3% of the invasive arm and 15.5% of the medical therapy arm. The secondary endpoints were also similar in both groups (CV death or MI was 11.7% and 13.9% and all-cause death was 6.4% and 6.5% of the invasive and medical therapy arms respectively). The hazard ratio for the periprocedural MI invasive/conservative was 2.98, 95% confidence interval (CI)1.87-4.74 and for the spontaneous MI was invasive/conservative 0.67, 95% CI 0.53-0.83).
The conclusion of the trial is that a routine invasive approach to patients with stable disease and moderate to severe ischemia failed to reduce major adverse cardiac events compared with optimal medical therapy alone.
So, if the results are so definitive why are the discussions and debates on going? Well it’s like car shopping. It’s not just about the color…do I want a sedan?..Is an electric car available in our area?..what is my budget?..Jaguar, Mustang, Camry.
Decisions are tailored to individual patients, individual centers, and individual healthcare systems. If a patient has stable disease with a depressed systolic function, ISCHEMIA is not applicable as a left ventricular ejection fraction <35% was an exclusion criterion as was advanced kidney disease with an estimated glomerular filtration rate <30 ml/min, prior CABG, and New York Heart Association class III-IV heart failure. Centers that don’t have a robust CCT program cannot use the ISCHEMIA protocol to screen patients with angina. Then there are those with occupational dilemmas, especially pilots and military personnel. Will a CCT to rule out left main disease be sufficient or will this pilot remain grounded until an invasive procedure is performed? Will the patient’s insurance cover a CCT, nuclear stress test and then possibly a coronary angiogram?
Presentations of landmark trials at conferences such as AHA ignite discussions that directly impact patient care, guidelines and future trials. The discussions drive the field forward. For interventional cardiologists, these discussions allow for much needed introspection. Unlike many other fields, interventional cardiology has always paved the road to randomized trials that on many occasions limit the inappropriate use eg COURAGE, ORBITA, and now ISCHEMIA. This is what distinguishes this subspecialty from many others.
Figure 1: ISCHEMIA Trial Design
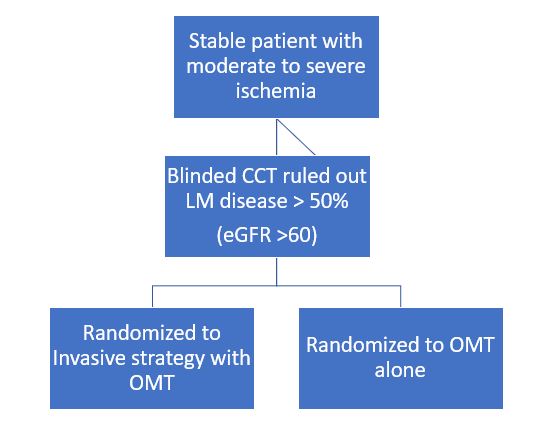
- Average Follow up 3.5 years
- Primary Endpoints: CV death, MI, resuscitated cardiac arrest, hospitalization for unstable angina or heart failure
- Secondary Endpoints: CV death, MI, angina QOL
The views, opinions and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your personal health matters. If you think you are having a heart attack, stroke or another emergency, please call 911 immediately.