During the AHA’s Scientific Session 2021, heart health, defined by the Life’s Simple 7 metric, was often woven into health equity conversations.

Empirical evidence consistently supports AHA’s recognition of these seven risk factors that people can avoid or improve on through lifestyle changes to help achieve ideal cardiovascular health. Regardless of how challenging this goal is for the average American, Life’s Simple 7 is an essential benchmark for staying heart-healthy.
 More attention is now being directed at the role of sleep in maintaining heart-healthy lifestyle practices. Sleep plays an important role in overall health and well-being. In-kind, there exists a reciprocal relationship between the quality of one’s diet, physical activity, and stress on the quality of sleep achieved. Ideally, sleep needs to be deep and restorative to support good cardiovascular health. Specifically, the Centers for Disease Control and Prevention recommend that adults between 18-65 years aim for at least seven hours of quality sleep per night. However, sleeping well is not common. 4 in 10 adults report consistently good sleep at night, and 50 million to 70 million American adults suffer from chronic sleep problems or sleep disorders.
More attention is now being directed at the role of sleep in maintaining heart-healthy lifestyle practices. Sleep plays an important role in overall health and well-being. In-kind, there exists a reciprocal relationship between the quality of one’s diet, physical activity, and stress on the quality of sleep achieved. Ideally, sleep needs to be deep and restorative to support good cardiovascular health. Specifically, the Centers for Disease Control and Prevention recommend that adults between 18-65 years aim for at least seven hours of quality sleep per night. However, sleeping well is not common. 4 in 10 adults report consistently good sleep at night, and 50 million to 70 million American adults suffer from chronic sleep problems or sleep disorders.
As an early career epidemiologist, who was not too long ago a pre-doctoral candidate, I am familiar with several factors that contribute to trouble with sleep. These have included staying up late to work on an analysis or drafting a manuscript whose internal deadline was already past due; following up on emails while binging a popular streaming series and munching on some snacks; juggling a busy household with two young children that always find a reason to wake up sometime after midnight. Perhaps these experiences are relatable. Often lifestyle choices, poor sleep habits, stress, and medical conditions can play a role in why you can’t sleep.
Alcohol
- A glass of wine before bed might not interfere with your ability to drift off but indulging in more servings of alcohol before bedtime may impair your sleep by interfering with your sleep cycle, especially REM sleep. This leads to fragmented, unrefreshing rest.
Poor Sleep Habits
- Habits that make it harder to fall and stay asleep may include (1) staying up late, (2) watching television in bed, (3) playing or browsing on your phone in bed, (4) having an irregular sleep schedule. Simple lifestyle changes to your nightly routines could help to remedy these issues.
Bed Sharing
- Whether with a partner, child, or pet, reduced sleep quality can be caused by sharing your bed. Anything that can make you uncomfortable (i.e., snores, crowding, pulled covers, or mismatched sleep condition preferences like temperature, light, or noise level) will disrupt your sleep.
Poor Sleep Environment
- Sleeping environments that are too hot or too cool will disrupt your sleep. Sleep experts recommend a bedroom temperature at a moderate climate between 65 to 72 degrees Fahrenheit at night. The body needs to cool at night for the most refreshing sleep, but a too-cold room will cause you to wake up. Don’t forget about light exposure. Whether it’s from a reading lamp, television, streetlight, or even the glow from a device, this could be enough to signal your brain to wake up.
Caffeine
- Some folks may argue that coffee has no effect on their ability to sleep at night and will enjoy a cup before bed. However, caffeine has a half-life of three to five hours, so even a late afternoon caffeinated beverage can disrupt your sleep later that night.
Stress
- Often the events of the day that creep back into our minds at night are not the positive experiences but the ones that fill our minds with worry and stress. Stress is one of the most cited symptoms of sleep problems.
Exercise
- Exercise, like an evening walk, is excellent for fostering better sleep. But intense, heart-pumping, and sweat-inducing cardio workouts within three hours of your bedtime may be too much. Both your body temperature and heart rate naturally drop as you fall asleep. Exercise stimulates your entire nervous system and raises these two body functions making it difficult to sleep.
Snack Choices
- Snacks or meals high in fat or protein consumed right before bedtime can overstimulate your digestive system, cause heartburn and make it difficult to sleep. A late-night sugar rush can also lead to hunger pangs and drops in blood sugar, causing you to wake up.
Sleep Disorders and Mental Health
- Importantly other factors like sleep disorders and mental health problems can make it difficult to sleep. You should talk with your doctor if you suspect that a medical or mental health condition may be contributing to your poor sleep.
Insufficient sleep and poor sleep quality, in addition to sleep disorders, are linked to a wide range of adverse health effects. Major physical and mental health consequences include anxiety, bipolar disorder, hormone imbalances, weakened immune system, cardiovascular disease, and major heart disease risk factors like obesity, inflammation, Type 2 diabetes, high blood pressure. Additionally, poor sleep is linked to overall decreased quality of life and increased mortality risk.
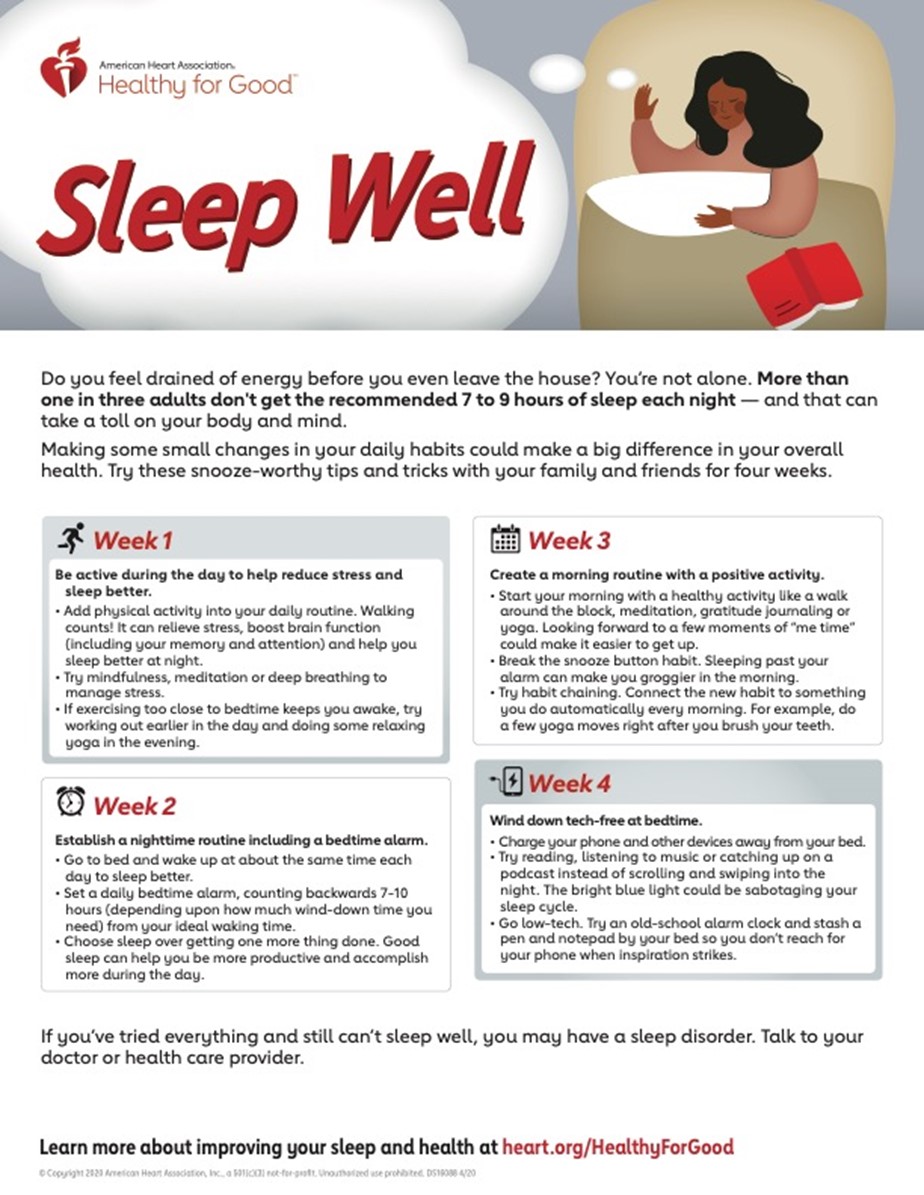
If good sleep habits are not currently part of your daily routine, consider some useful strategies to alleviate some of the factors that have interfered with your quality and quantity of sleep. Here in this infographic are a few tips and techniques developed by AHA to help those who do not have a sleep disorder make small daily changes to establish healthier sleep habits.
Working to alleviate factors that contribute to insufficient sleep and poor sleep quality may also be another critical metric for cardiovascular health. Preliminary findings presented at the AHA’s 2021 Epidemiology and Prevention/Lifestyle and Cardiometabolic Health Scientific Sessions recommended revising the AHA’s Life’s Simple 7 to include sleep as a metric creating a new “Simple 8 or Essential 8” metric measuring cardiovascular health. The study’s lead investigator, Nour Makarem, Ph.D., explained that while sleep is a health behavior that people engage in every day, like diet and exercise, it has received far less attention. However, increasing evidence links sleep to heart disease and risk factors for cardiovascular disease.
Along with her team of investigators, Dr. Makarem assessed whether a cardiovascular health score that includes the Life’s Simple 7 combined with sleep metrics would be more strongly associated with cardiovascular disease than the Life’s Simple 7 score. The study found that when at least one measure of sleep was added with the Life’s Simple 7 measures, the new heart health score was more strongly associated with cardiovascular disease than the traditional Life’s Simple 7. The results were compelling and showed, for example, that study participants who received seven to eight hours of sleep a night in addition to meeting Life’s Simple 7 guidelines had up to 61% lower odds of having heart disease. Those who got less than six hours of sleep scored lower for overall cardiovascular health and had a higher prevalence of overweight and obesity, Type 2 diabetes, and high blood pressure. Sleep duration and the other sleep metrics included in the study made the cardiovascular health scores more predictive of cardiovascular disease risk than the seven metrics alone.
Like several current Life’s Simple 7 measures, clocking 7-9 hours of sleep per day can be challenging. However, the traditional cardiovascular health metric may need to be revisited for a potential upgrade in providing yet another vital benchmark for predicting and promoting ideal cardiovascular health.
References:
- Lloyd-Jones, Donald M., et al. “Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond.”Circulation 4 (2010): 586-613.
- https://www.heart.org/en/health-topics/sleep-disorders/sleep-and-heart-health
- https://www.heart.org/en/news/2020/03/06/sleep-should-be-added-as-measure-of-heart-health-study-says
- https://www.verywellmind.com/reasons-for-not-sleeping-well-and-how-to-fix-350760
- https://www.heart.org/en/healthy-living/healthy-lifestyle/sleep/sleep-well-infographic
- https://www.ahajournals.org/doi/10.1161/circ.141.suppl_1.36
“The views, opinions and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your personal health matters. If you think you are having a heart attack, stroke or another emergency, please call 911 immediately.”