PET or MRI, that is the question – Part 2
In our previous blogs, we discussed ASL MRI to image abnormal blood vessels in Moyamoya patients. We looked at a study that compared MRI and PET images of normal and healthy people. In this blog, we will look at the application of ASL MRI on adult Moyamoya patients.
According to the latest study by Dr. Moss Zhao (AHA Postdoctoral Fellow, 2021), ASL MRI can detect impaired blood flow and circulation in Moyamoya patients without any radiation or contrast agents.
In this study, Dr. Zhao’s team enrolled nearly 30 adult Moyamoya patients without acute stroke or tissue infarcts in the brain. They scanned the brain of these patients using the advanced ASL MRI technique (multi-delay ASL) that were tested successfully on normal and healthy people before. Similar to the study designed in the previous blog, Dr. Zhao’s team collected both ASL and PET images from the Moyamoya patients at the same time before these patients underwent their bypass surgery. The results from this study were convincing that ASL can replace PET to characterize the pathophysiology of Moyamoya disease patients. The image in this blog shows the vessel occlusion and its impact on blood flow in a Moyamoya patient.
Another advantage of ASL is the elimination of contrast agents. In many MRI exams, patients need to receive a contrast agent (such as gadolinium) to enhance the image quality. However, the contrast agent can cause side effects and deposit in the brain. Although there is no evidence suggesting its impact on health, we should minimize the use of these contrast agents. In the same study, Dr. Zhao’s team also demonstrated that the advanced ASL can create images without contrast agents and that doctors favored the new ASL technique over the conventional contrast-based imaging method.
Taken together, ASL MRI will become more accessible to radiologists to diagnose Moyamoya disease without causing side effects to patients. The technique will allow safe, affordable, and fast for imaging to identify patients with a higher risk for stroke.
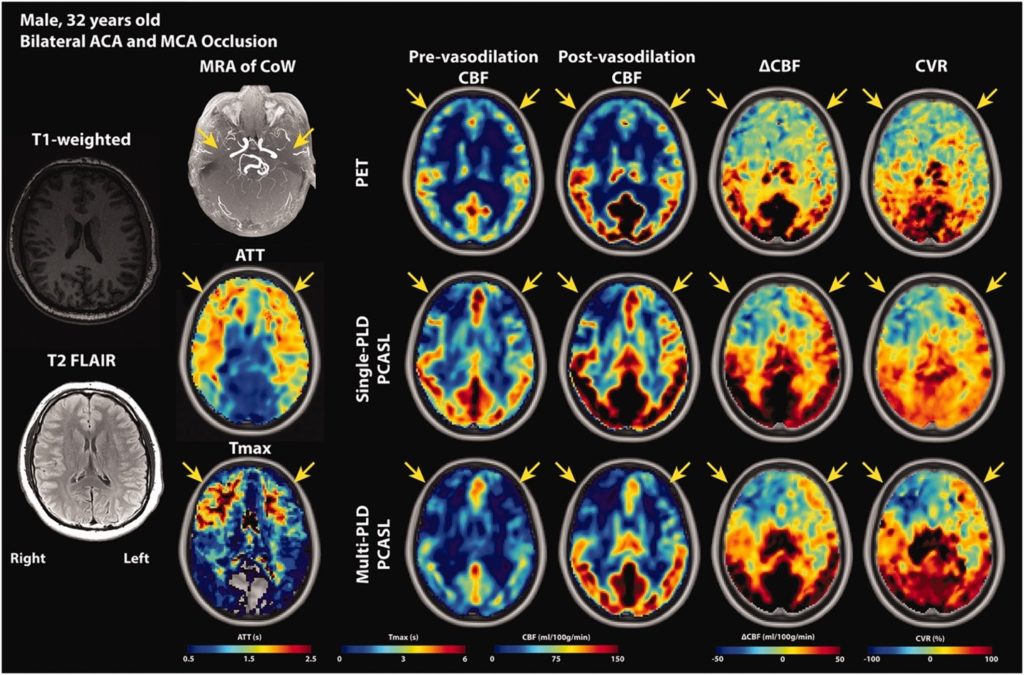
Image source: JCBFM
REFERENCE
https://doi.org/10.1177/0271678X221083471
“The views, opinions, and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness, and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions, or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your health matters. If you think you are having a heart attack, stroke, or another emergency, please call 911 immediately.”