The Health Costs of Hunger Part 2: What we can do about it
If you read my February blog, you know that food insecurity is a complex and overwhelming issue in the United States. In 2018, 37.2 million Americans were food insecure and of that, 6 million were children. The health consequences of food insecurity are significant and contribute to growing rates of chronic disease American’s have experienced in the past few decades. With recent changes to programs such as the supplemental nutritional assistance program (or SNAP), more Americans are at risk for becoming food insecure.
The lack of stable access to adequate safe food affects a persons’ health and well-being in profound ways. And as health care providers used to acting, we want to do something about food insecurity in our communities. But what can be done and where to start? To answer these critical questions, I spoke with Alissa Glenn, consultant of food as medicine program at the Greater Cleveland Food Bank, who offered this advice.
- Acknowledge that food insecurity is pervasive and talk about it. Hunger affects people of every gender, age, race and ethnicity throughout the United States. Yet, an important reason people often do not pursue supportive programs such as SNAP, is the longstanding stigma around assistance. One of the best ways to break this stigma is by talking openly and compassionately about food insecurity in your community.
- Educate yourself and your colleagues. My February blog, had a lot of scientific resources on food insecurity hyperlinked. Last year, the AHA published a science advisory on innovative strategies to create a healthy and sustainable food system that can provide useful context. In addition, lay resources such as the Feeding America website and books like Stuffed and Starved can help explain this complex issue. Finally, consider inviting your local food bank to conduct a continuing education or a Grand Rounds session on addressing food insecurity in clinical settings. They can describe local resources in your own community and practice poverty simulations to help healthcare providers feel more comfortable discussing food insecurity with patients.
- Ask your patients about it. Screening for food insecurity is recommended by groups such as the American Association of Pediatrics which suggests incorporating such a screening at every patient visit.
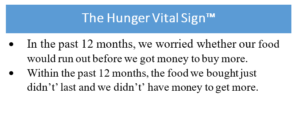 I know, we have to fit so much into each patient encounter that trying to fit in one more thing seems impossible. But a quick, simple strategy is to administer the Hunger Vital Sign™ (Left Insert).
I know, we have to fit so much into each patient encounter that trying to fit in one more thing seems impossible. But a quick, simple strategy is to administer the Hunger Vital Sign™ (Left Insert).
It can be hard for patients to acknowledge they are food insecure so helping them feel comfortable can result in more honest answers. Best practices include asking screening questions after the patient has been with the provider for a while, having a team member with a longstanding relationship ask screening questions, and if possible, to ask them via tablet or computer to reduce awkwardness.
- Refer patients and family members who are food insecure and may need immediate help to local resources. This can include local food pantries, produce distribution sites, hot meals, and perhaps, onsite therapeutic food clinics. If your clinical setting is lucky enough to have to have a registered dietitian, involve them in developing a list of local resources to be distributed to patients. Case managers and outreach workers can also provide patients resources about short and long-term support for food insecurity. To find a food bank near you, please check out the Feeding America
- Advocate for anti-hunger programs. SNAP is the first line of defense against food insecurity. For every meal that a food bank provides, SNAP provides 9 meals. As the largest effort to address hunger in the U.S., changes to this program that reduce eligibility or benefits will increase the number of hungry Americans. Working with your community and engaging with your elected officials about how hunger influences the health care you provide are powerful ways to advocate for their continued support. To find out more about advocating for SNAP and the Child Nutrition Reauthorization Act, please review the Advocating for a Hunger-Free America
- Use your professional associations. As healthcare professionals, we have a powerful voice. Every day we talk with dozens of patients and family members about how to improve their health and well-being. As you get more comfortable talking with your patients talking about food insecurity, you will likely hear stories about how hunger affects their health. Work with your professional associations to collect those stories and with one voice advocate for changes in practice, education, and policy.
Last month, the AHA released its 2030 Impact Goal. This ambitious statement recognized the importance of structural changes to achieve a world of more equitable, longer, healthier lives. It creates a framework from which professional organizations can harness the energy and experience of its members to initiate conversations about food insecurity, incorporate food insecurity education into the training of providers, increase food insecurity screening in clinical settings, and use the collective voice of 40 million volunteers and members to effectively advocate for anti-hunger programs.
There are many ways you can work with the AHA to reduce food insecurity in America. Consider working with your scientific council to propose a scientific statement on the effects of food insecurity on cardiovascular health, propose a workshop on clinical food insecurity protocols at a Scientific Sessions meeting, or write an editorial on your experiences helping a patient with food insecurity. The enormity of hunger in America, and its deleterious effects on the health of our patients, can be overwhelming. But even small steps such as reading a book on food insecurity, screening patients in your clinic, or advocating for structural change, can be powerful ways to help to reduce food insecurity.
“The views, opinions and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your personal health matters. If you think you are having a heart attack, stroke or another emergency, please call 911 immediately.”