Fighting for Health Equity and Social Justice during the COVID-19 pandemic: Insights from the 2021 Epi/Lifestyle Scientific Sessions
This year’s Epi/Lifestyle Scientific Session took place on May 20-21, 2021. Despite the change in venues to virtual mode because of the COVD-19 pandemic, the conference was a success! Many attendees had the opportunity to participate, network, and learn about the latest science on Epidemiology, prevention, lifestyle, and cardiometabolic health. The opening remarks and keynotes centered on two particularly important topics, health equity, and social justice, and the commitment of the American Heart Association to eliminate health disparities in underserved ethnic communities.
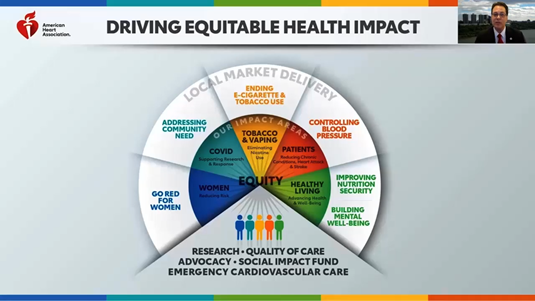
Dr. Mitchell S. V. Elkind, MD, MS, FAAN, FAHA, American Heart Association President, opened the conference, highlighting the commitment of the American Heart Association to health equity and structural racism research, driving systemic public health change, while focusing on removing barriers to equitable health for everyone, everywhere. He also provided updates on new scientific research programs to address health inequities and structural racism, and diversity research opportunities for underrepresented racial and ethnic groups.

From a healthcare provider standpoint, many of these programs offer opportunities to bridge the gap in preventive CVD measures in our communities. Other important contributions highlighted at the conference included the COVID-19 Registry, a hospital-based quality improvement program to explore the links between COVID-19, cardiovascular risk factors, and adverse cardiovascular outcomes.
In alignment with the lead topic of the conference, two keynote speakers, Dr. Olajide A Williams and Dr. Laprincess C. Brewer highlighted the effects of structural racism on the social determinants of health, and their relation to health equity and social justice. Dr. Olajide A. Williams presented on the relationship between structural racism and poor health. He highlighted the importance of social determinants of health and primordial prevention from the perspective previously reported by Dr. Camara Jones.1
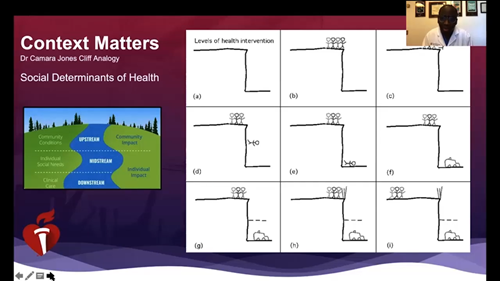
Dr. Jones’ “Cliff Analogy” gives a clear picture of the three dimensions of health interventions to help people who are falling off of the cliff of good health: providing health services, addressing the social determinants of health and equity.1 The deliberate movement of the population away from the edge of the cliff represents our efforts to improve on the social determinants of equity through interventions on the structures, policies, practices, norms, and values that differentially distribute resources and risks along the cliff. By doing so, we can improve health outcomes and eliminate health disparities.1 His presentation is also a call to continue efforts to overcome the long-term effects of structural racism and eliminate its associated disparities by organizations outside of government.
Another keynote speaker, Dr. Laprincess C. Brewer discussed the importance of community-based participatory research as a strategy to promote cardiovascular health for all. She highlighted the importance of diversity in clinical trials and research studies as well as the need to build and maintain community partnerships to dismantle structural inequities, racism, and consequently lead to cardiovascular health equity in our communities. Innovative approaches through community-based participatory research, involving our communities and key stakeholders have the potential to support lifestyle change for cardiovascular disease (CVD) prevention, especially in ethnic minority groups, such as African Americans, who carry the largest CVD burden.
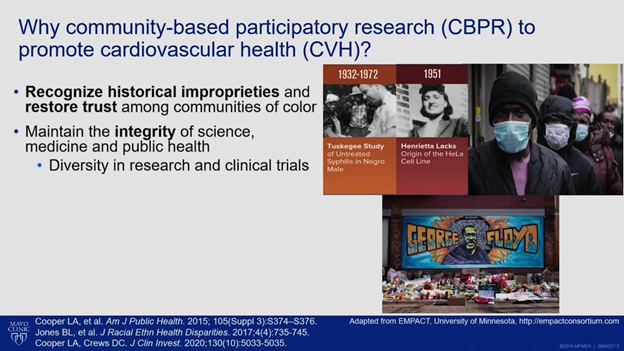
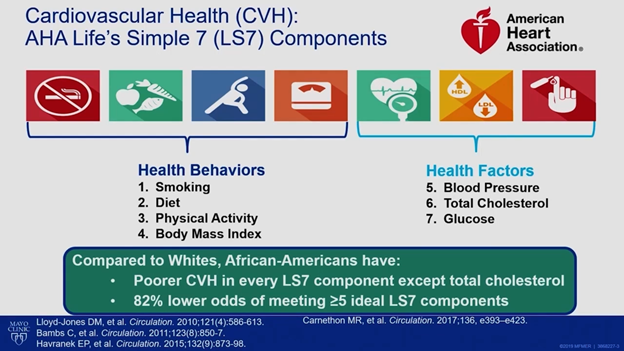
Dr. Brewer highlighted the ongoing disparities in CDV mortality for African Americans. Despite improvements in mortality rates over the past decades, CVD remains the leading cause of death for African-Americans. She further messaged the American Heart Association’s Life Simple 7 as important factors to address in the fight against cardiovascular disease in ethnic minorities experiencing greater health disparities. Her presentation also highlighted the importance of community stakeholders, including faith-based organizations and community members in the identification of the research problem, development of research questions, as well as interventions that may be relevant to these groups.2 The various types of programs she discussed, including Mobile Health, emergency preparedness, and COVID testing, through a partnership with a faith-based organizations, served as examples of trusted social networks and established stakeholders that underserved communities may be more likely to reach out for support during health crises. These may further contribute to the delivery of culturally sensitive resources through community partnerships aimed to achieve health equity among ethnic minorities.
As I reflect on the message from the speakers during the opening session, it reminds me of the opportunities available in my community for engagement in the prevention of CVD, especially in underserved minority groups, and the need to reach out to key stakeholders trusted by these underserved groups. It is also a call to engage with these stakeholders in the delivery of interventions aimed at disease prevention, setting up guardrails to prevent them from falling off the cliff of good health.
References
- Jones CP, Jones CY, Perry GS, Barclay G, Jones CA. Addressing the social determinants of children’s health: a cliff analogy. J Health Care Poor Underserved. 2009;20(4 Suppl):1-12. doi:10.1353/hpu.0.0228
- Brewer LC, Hayes SN, Caron AR, et al. Promoting cardiovascular health and wellness among African-Americans: Community participatory approach to design an innovative mobile-health intervention. PLoS One. 2019;14(8):e0218724. Published 2019 Aug 20. doi:10.1371/journal.pone.0218724
“The views, opinions and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your personal health matters. If you think you are having a heart attack, stroke or another emergency, please call 911 immediately.”
 Whether or not scientists should blog has been hotly debated. In 2018, Eryn Brown and Chris Woolston published a
Whether or not scientists should blog has been hotly debated. In 2018, Eryn Brown and Chris Woolston published a 




 Dr. Emelia Benjamin utilizes the theories from Kathy Kram, Monica Higgins, and David Thomas on “Creating Developmental Networks” and “Reconceptualizing Mentoring” with her early career faculty at BU. Take a cue from her, and use this worksheet,
Dr. Emelia Benjamin utilizes the theories from Kathy Kram, Monica Higgins, and David Thomas on “Creating Developmental Networks” and “Reconceptualizing Mentoring” with her early career faculty at BU. Take a cue from her, and use this worksheet, 


