ECPR: What is it? And what do we know in 2020?
Despite advances in the resuscitation field, cardiac arrest, especially cardiac arrest in the setting of cardiogenic shock, continues to carry significant morbidity and mortality. This topic continues to challenge healthcare providers on ways to improve outcomes in patients with refractory cardiac arrest. Extra-Corporeal Membrane Oxygenation (ECMO) is a type of mechanical circulatory support device utilized for various conditions, including cardiogenic shock and multi-organ failure. I heard about ECPR recently, so I wanted to share what is out there, and potentially motivate colleagues and professionals to share their thoughts on this important topic.
What is ECPR?
ECPR (Extra-corporeal Cardio-Pulmonary Resuscitation) is the implementation of ECMO in selected patients with cardiac arrest, and may be considered when conventional CPR efforts fail in a setting with expeditious implementation and support.by skilled providers When/where does ECMO cannulation occur in these patients?
Patients with cardiac arrest and ongoing CPR are transported to the hospital while ongoing resuscitation efforts are being taken. ECMO potentially provides the circulatory and respiratory support these sick patients need until reversible conditions are addressed. ECMO cannulation usually occurs at the healthcare center, where skilled personnel and healthcare providers have expertise in ECMO. Figure 1 shows a simple illustration veno-arterial VA-ECMO utilized in ECPR.
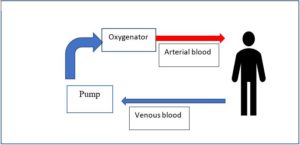
Figure 1: Simple schematic illustration of veno-arterial VA-ECMO utilized in EPCR.
What is the scientific evidence for the use of ECPR?
Unfortunately, there are no randomized controlled trials (RCTs) on the use of ECPR in cardiac arrest patients at this time. The evidence supporting ECPR comes from observational studies in the past two decades, in patients with out-of-hospital cardiac arrest, and studies looking at ECPR in in-hospital cardiac arrest. Many, but not all, of the observational studies showed overall favorable neurological outcomes in those who receive ECPR compared to conventional CPR. It is important to note, however, that these studies had variable inclusion criteria, and potential risk for confounding bias, making their validity and generalizability questionable.
Are there any AHA guidelines supporting the use of ECPR?
AHA 2019 Guidelines Updates:
Recommendations—Updated 2019
- There is insufficient evidence to recommend the routine use of ECPR for patients with cardiac arrest.
- ECPR may be considered for selected patients as rescue therapy when conventional CPR efforts are failing in settings in which it can be expeditiously implemented and supported by skilled providers (Class 2b; Level of Evidence C-LD).
Why is this important?
Some studies in the past 2 decades have shown that ECPR might be associated with favorable neurological outcomes compared to conventional CPR. It is known that neurological outcomes in cardiac arrest patients have a significant effect on morbidity and mortality. As such, although these are observational studies with limited evidence, they shed light on a potential therapy that could lead to better outcomes in this very sick population. Future studies, including RCTs, are much needed to assess the outcomes of ECPR and identify patients who would benefit the most from this potential therapy.
I would like to say special thank you to my friend and colleague, Dr Khaldia Khaled, for her help on this blog.
Reference
Panchal et al: 2019 American Heart Association Focused Update on Advanced Cardiovascular Life Support: Use of Advanced Airways, Vasopressors, and Extracorporeal Cardiopulmonary Resuscitation During Cardiac Arrest: An Update to the American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2019;140:e881–e894. DOI: 10.1161/CIR.0000000000000732.
The views, opinions and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your personal health matters. If you think you are having a heart attack, stroke or another emergency, please call 911 immediately.