The Era of Misinformation: A Constant War of Science vs. Fiction
“Covid19 is a hoax”, “vaccines poison your body”, “the earth is flat.” Various conspiracy theories and misinformation statements have existed throughout history. Though some might seem absurd and often put into the spotlight to ridicule them as they are improbable to be accurate, like the earth being flat, this comedian aspect shifts to a sinister black connotation when the conspiracy theories, and misinformation infect the medical field.
As the first doctor of my family, it is not uncommon to get questions about a new drug that was promoted on TV, or regarding a bold scientific claim, such as someone curing cancer. However, during this year, amid the Covid19 pandemic, the spread of misinformation has been almost as incontrollable as Covid19 cases in the United States of America. With great concern, I saw that several acquaintances, friends, and family, most of them with higher education degrees, shared and contributed to spread false information on the treatment of Covid19, its origin, or questioning if this was part of a bigger plot to control humanity.
The spread of misinformation has contributed to mistrust towards medical healthcare personnel, to the point of being violent towards them,1 not following their advices, or falsely claiming overdiagnosis of Covid19 with the sole purpose of getting “more money,” claim that unfortunately gets backed up by the Highest Office in the Land.2
However, this problem isn’t new in the medical community, as Dr. Anne Marie Navar stated in her conference during the Scientific Sessions lecture “How Misinformation Steers Patients off Course.” She mentions that the Covid19 pandemic highlighted and made more evident the dire problem misinformation has brought to medical compliance with treatments. She focuses on the misinformation campaigns that have been occurring around statins, were social media personalities with doubtful medical claims such as the questionable Dr. Joseph Mercola, and unscrupulous social medial like Infowars pretend to scare and deter patients from taking statins, while promoting their products such as diets, supplements (Omega-3), that are commercialized with misleading labels, and lies about the efficacy of their products.
But how likely are statements made by doubtful doctors or non-healthcare providers likely to affect patient compliance? Would patients believe more something they read or see on social media than following the physician’s recommendations to whom they trust their health? Unfortunately, it is quite likely. Dr. Navar highlights a prospective cohort study from Denmark that included 674.900 individuals > 40 years old, that were on statin therapy ( a drug used for patients with high cholesterol levels) from 1995-2010, and followed until December 31 of 2011, to test the hypothesis if statin-related news were associated with early statin discontinuation.3
This prospective cohort showed that early statin discontinuation increased with negative-statin related news, and early discontinuation was associated with increased risk of myocardial infarction and death from cardiovascular diseases (fig 1). Also, a sensitivity analysis showed that negative statin-related news stories were associated with an odds ratio of 1.15 (CI: 1.09-1.21) for early discontinuation of antihypertensive medication (fig 2).3
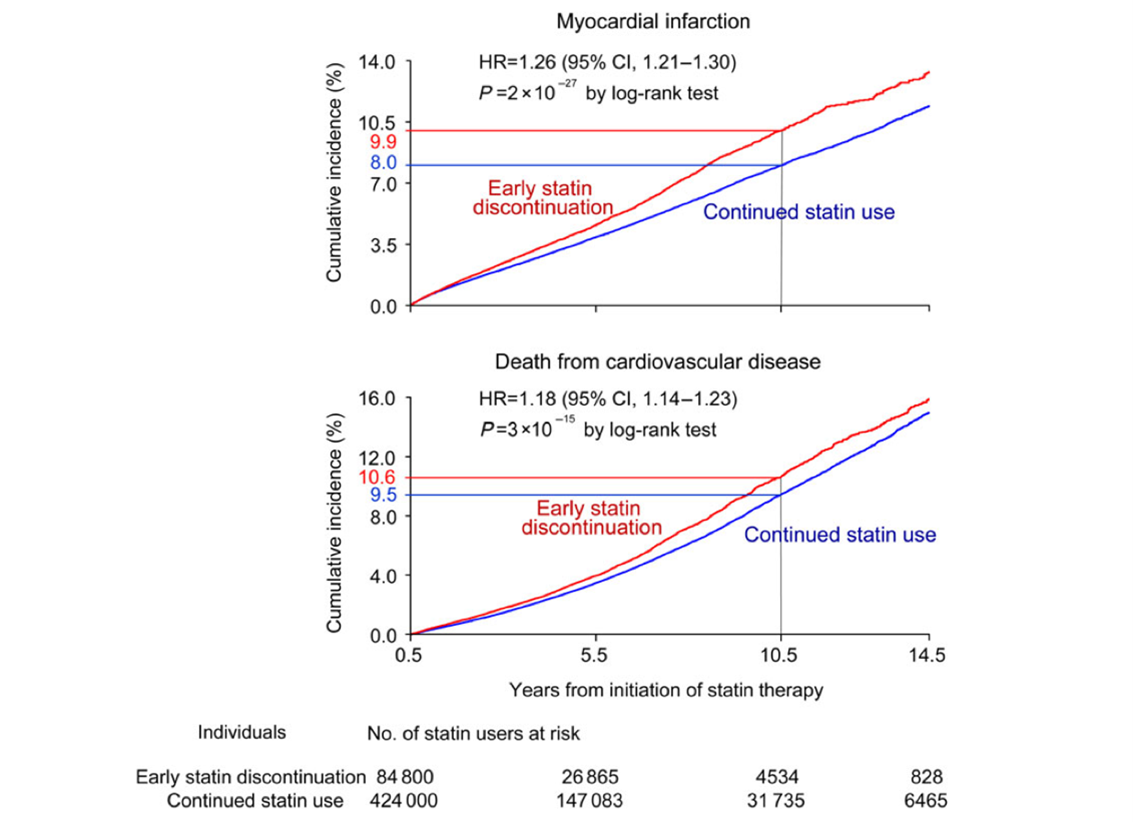
Fig 1. Early statin discontinuation vs. continued use and cumulative incidence of myocardial infarction (top panel) and death from cardiovascular disease (bottom panel).
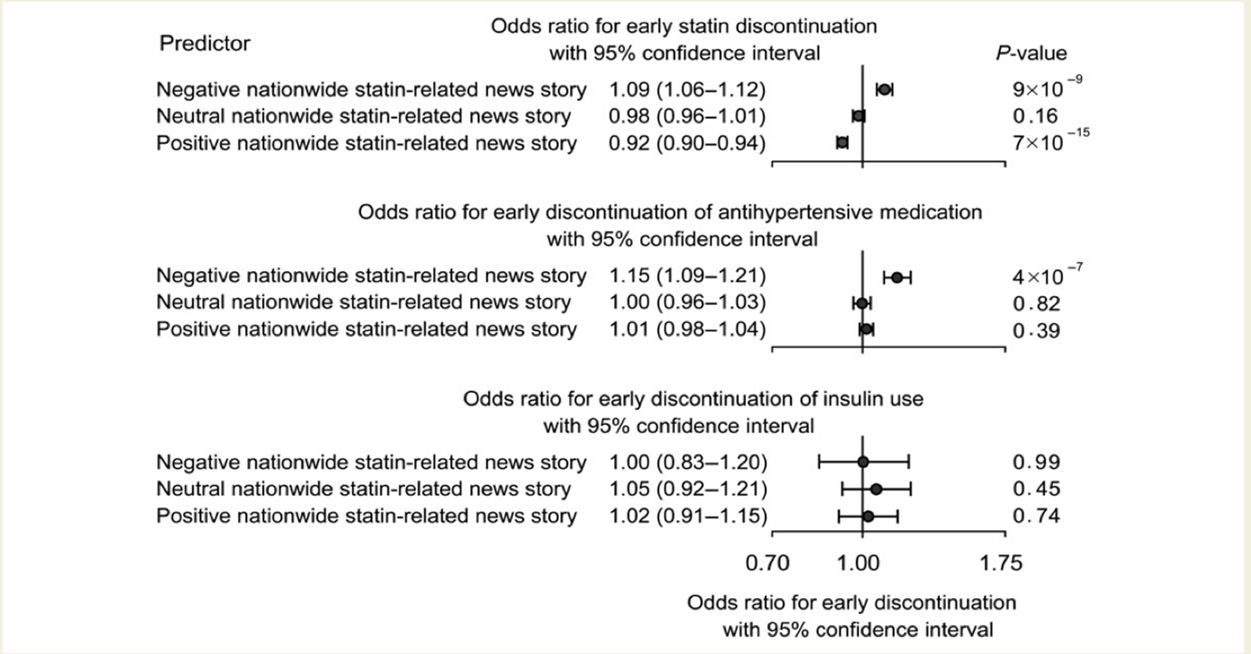
Fig 2. Statin-related news stories and early discontinuation of statin, antihypertensive medication, and use of insulin among statin users.
It is worrisome that patients’ very own life might be at stake due to misleading propaganda that feeds from the fear of exaggerating adverse events for specific treatments (drugs, vaccines, etc.). To have these very own propaganda makers, in an ungracious second act, pretending to be messiahs, to promise patients the “healthiest” option available for their disease, thus creating widely successful businesses by selling non-effective products at the expense of putting the populations’ health at risk.
But this misinformation phenomenon has been more impactful and dreadful during the pandemic since we are dealing with a highly transmissible disease, where the cost of disinformation results in more people getting infected with Covid19 ,or dying because of Covid19.
But what can we do as healthcare professionals? As scientists? The first thing to do is to speak up. We must not be silent as false and misleading information spreads. The truth tends not to be soothing, hopeful, nor easy to process, and during this cumbersome year, this might become a more challenging task when coming to terms with “the new normal.” The evidence does not change because of our feelings, thus making it imperative to face the facts. Our role as physicians, healthcare workers, and scientists is to be modern versions of Prometheus, and reside on the frontline to fight back misinformation by being leaders that defend the torch truth, and share it with the world.
Dr. Anthony Fauci is the perfect example of the leadership we all must show as bearers of the torch of truth, as his statements are based on hard facts and science. Nonetheless, his remarks often failed to reassure people during these unprecedented times since he has been very cautious by avoiding making any premature conclusions regarding the effectiveness of a treatment or on the efficacy of a vaccine without proper evidence, as it should be.
However, this lack of reassurance opens a door for opportunistic scientists and medical doctors such as America’s Frontline Doctors, that earlier during the year claimed that Covid19 could be treated with hydroxychloroquine, widely tested as being not useful.4,5 This bold claimed amid the uncertainty lived in the beginning of the pandemic, unleashed an incontrollable confirmation bias, as people would feel reassure when “doctors” tell them there is a cure for this virus; despite the fact that the “doctors” making such claims were not infectious disease experts, nor did they have any real evidence to support those claims. This mere example highlights the importance of raising our voices to spread real facts to prevent landslides of false information spread.
We must be empathetic to those that are sharing or commenting on false information. When seen friends or family doing this, please give them the benefit of the doubt, as people share information thinking of their well-being and that of others and, most of the time, is not out of a primary motive to harm or do wrong. When I have encountered my family or friends doing this, I try to reach out to them and ask them what they learned from the information they are sharing and explain to them the inaccuracies of all the misleading content on the news they are spreading. At last, I tell them to send me privately all the videos, chats, news they get so we can discuss them before sharing them. By doing this, the fake news chain will break, and more people will start acquiring critical thinking before sharing news from a field that is unknown or unfamiliar to their area of expertise, in this case, medical and healthcare related news.
Finally, I would like to share a pamphlet on how to fight misinformation from Dr. Tim Caufield from the University of Alberta that outlies four main steps, help stop the spread, and craft a message to counter misinformation, promote a regulatory response, and debunking (fig 3). Let us all unite our voices so they can be loud enough to bury misinformation.
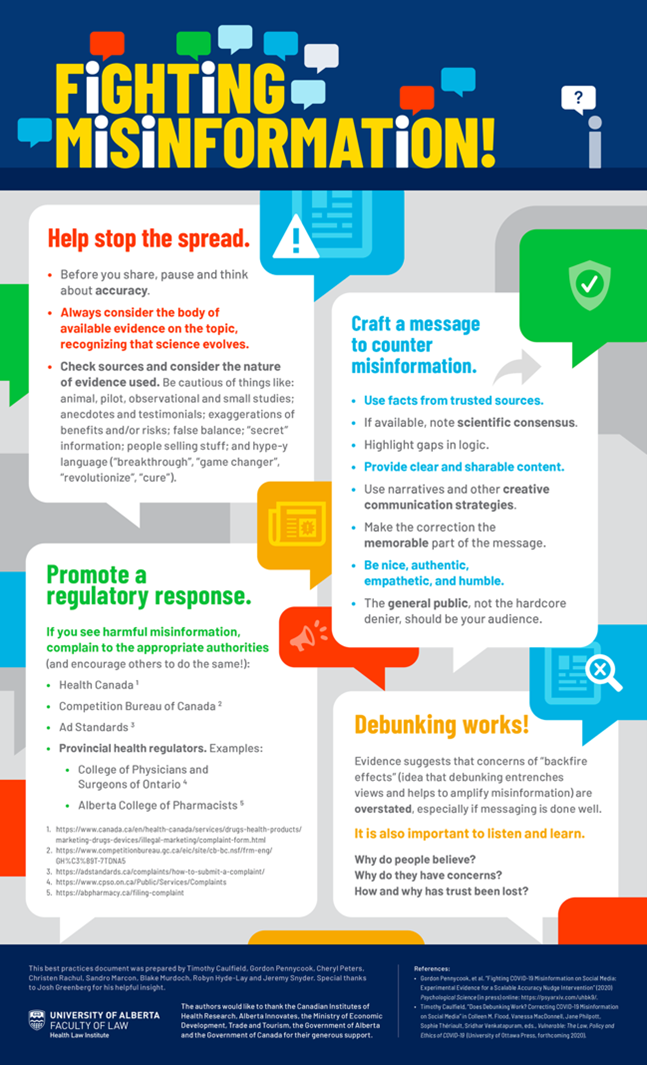
Fig 3. Fighting misinformation pamphlet (https://www.ualberta.ca/law/faculty-and-research/health-law-institute/fighting-misinformation.html)
Acknowledgments
I would like to thank Dr. Anne Marie Navar for her conference “How Misinformation Steers Patients off Course” As it encouraged me to write todays blog on this pressing issue. I encourage you all to see her conference on the Scintific Sessions website.
References
- Medellin. Personal médico del Hospital General fue agredido por caso de covid-19. El Tiempo. https://www.eltiempo.com/colombia/medellin/coronavirus-en-medellin-denuncian-agresion-a-personal-medico-del-hospital-general-de-medellin-527090. Published 2020. Accessed.
- Griffin J. Medical professionals push back after Trump says COVID-19 cases are inflated to ‘get more money’. Daily Herald 2020.
- Nielsen SF, Nordestgaard BG. Negative statin-related news stories decrease statin persistence and increase myocardial infarction and cardiovascular mortality: a nationwide prospective cohort study. Eur Heart J. 2016;37(11):908-916.
- Boulware DR, Pullen MF, Bangdiwala AS, et al. A Randomized Trial of Hydroxychloroquine as Postexposure Prophylaxis for Covid-19. New England Journal of Medicine. 2020;383(6):517-525.
- Effect of Hydroxychloroquine in Hospitalized Patients with Covid-19. New England Journal of Medicine. 2020.



 this year, I have gathered some advice from my Cardiology fellowship program director (
this year, I have gathered some advice from my Cardiology fellowship program director (