Hopes for 2021
As 2020 concluded with all of the unprecedented events, with the tragedies people had to suffer and are still suffering from, with all the good and bad, we enter the New Year of 2021 with some hope; hoping for better health, better strategies to combat what we are dealing with in this pandemic, and being more responsible for each other.
COVID-19 Pandemic
COVID-19 pandemic has changed how we live our lives, and the impact of this pandemic will likely last at least a few years, if not more after the pandemic is over. There are a lot of “unknowns” about COVID-19 infection, including the long-term effects of this infection and the effectiveness of some medications, that we will get to encounter and manage in the next several years.
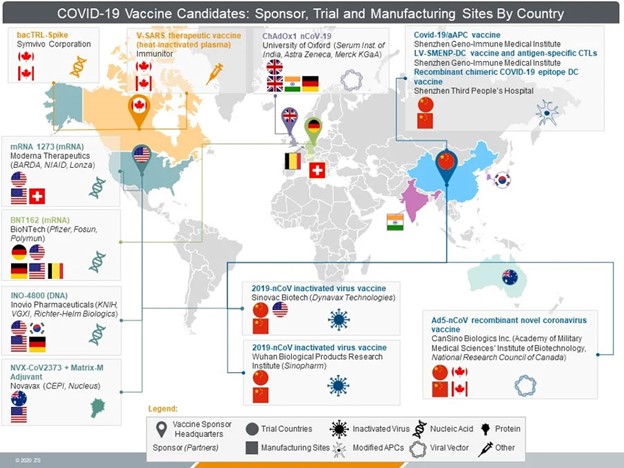
COVID-19 Vaccine
With multiple effective vaccines discovered recently, healthcare workers were given priority to get the vaccine, followed by more vulnerable patients, including the elderly and those with significant comorbidities. The Centers of Disease Control and Prevention (CDC) website provides helpful information on the currently available vaccines in the United States (US), Pfizer, and Moderna, including their storage, preparation, and expected side effects (Link is provided below) [1]. The hope is that by the Spring of 2021, 75% of the population in the United States will be vaccinated. Moreover, efforts by international organizations, including the World Health Organization (WHO), to distribute the vaccine to all countries are ongoing [2].
COVID-19 New Strains
We have seen the discovery of new strains of COVID-19 infection in the United Kingdom and, most recently, the US. These new mutant strains of COVID-19 may not be covered by the available vaccines, as such, the vaccine is an additional layer of protection, with the other protection measures, including social distancing, masks, and hygiene, which may be the most important way to prevent the spread of these new strains at this point of time.
With all that being said, our hopes for a “normal 2021” depend on how we handle the COVID-19 pandemic, we may not see everything going back to normal in 2021, but we can work on making the initial right steps now so that we have less grief, less “loss,” fewer travel restrictions, with healthier and happier upcoming years!!
Special thank you to my sister, Rawan Ya’acoub, an assistant professor of Doctor of Pharmacy/Clinical Pharmacology at the University of Jordan in Amman, Jordan, who helped me write this blog, and for all of her support.
References
- S. COVID-19 Vaccine Product Information: https://www.cdc.gov/vaccines/covid-19/info-by-product/index.html
- COVID-19 vaccines: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/covid-19-vaccines
“The views, opinions and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your personal health matters. If you think you are having a heart attack, stroke or another emergency, please call 911 immediately.”