Importance of Physician Well Being in Today’s Practice Environment
Introduction
Each year in the United States, we lose talented physician colleagues to suicide1 and we are left asking ourselves how could this have been avoided. Over the last few years there has been an increasing focus on physician well being and avoiding physician burnout within the medical community. This endeavor in raising awareness within the medical community has extended to national medical meetings with focused sessions on physician well being. It is often perceived that this problem is not extensive and does not impact patient care. However, research in this area has provided data that dispels these myths. It has been shown that physician burnout had reached an all time high in 2014 affecting over 50% of physicians in some series and data has actually shown that physician burnout negatively affects patient outcomes2.
In this month’s blog, I will outline the latest statistics on the prevalence of physician burnout, the causes of physician burnout, signs of physician burnout, the impact of physician burnout on the healthcare system and will conclude on proposed methods for avoiding physician burnout.
Prevalence of Physician Burnout
The prevalence of physician burnout has been quoted as being as high as 54% in 2014 in a study led by Shanfelt, et al2. Burnout also affects female physicians greater than their male counterparts3. The problem with burnout is not confined to attending physicians but starts early in medical school and continues through residency and fellowship training3. In a study led by Shanafelt, et al it was shown that burnout was most prevalent in the 55-64 year old age group and least prevalent in the > 65 year old age group4. With regards to physician specialty, it was found that burnout was most prevalent in specialty physicians compared with primary care providers4. It is also more prevalent for physicians in surgical specialties versus non-surgical specialties4. Physician burnout is also highly prevalent for physicians on the frontlines in specialties such as Internal Medicine, Emergency Medicine, Family Medicine and Obstetrics and Gynecology3.
Definition and Signs of Physician Burnout
In 1974 Clinical Psychologist, Herbert Freudenberger defined burnout as exhaustion resulting from “excessive demands on energy, strength, or resources” in the workplace, characterizing it by a set of symptoms including malaise, fatigue, frustration, cynicism, and inefficacy3. Freudenberger further expanded on this definition to state that burnout usually occurs in the context of an increased demand on personal involvement and empathy with increased susceptibility in very dedicated and committed individuals3. This suggests that our very best physicians who are very conscientious about their work are susceptible to burnout which has great implications with regards to very talented physicians leaving their institutions and sometimes even exiting the field all together. There may be physical manifestations of burnout such as extreme emotional responses to feeling overwhelmed such as crying or yelling with extreme anger3. Other symptoms of burnout may also be persistent headaches, insomnia and resulting sleep deprivation and its consequences, lingering cold like symptoms, gastrointestinal symptoms, extreme exhaustion and shortness of breath3.
More recently, Christina Maslach developed a model of burnout which consists of three components, which include emotional exhaustion, depersonalization, and a diminished sense of personal accomplishment3. The Maslach Burnout Inventory (MBI), was later proposed and is composed as three subscales to measure the extent of an individual’s symptoms along each of the three components3. The MBI is the most commonly used tool to assess physician burnout3.
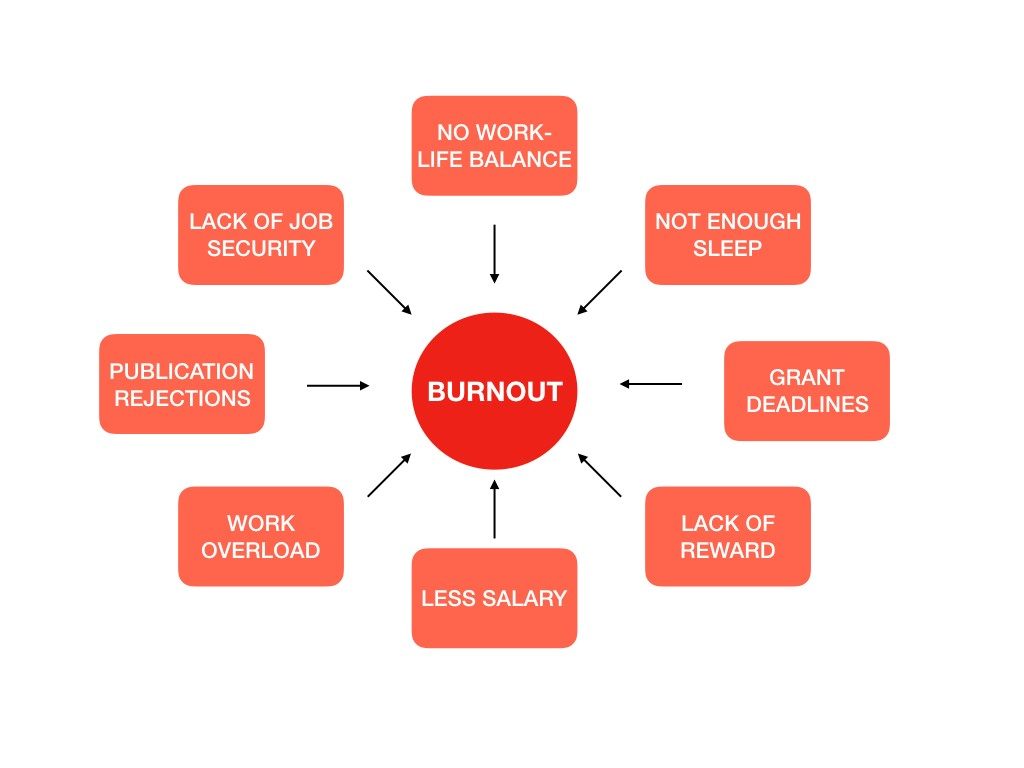
Causes of Physician Burnout
Surveys such as the Physician Life Inventory have identified three main contributors to physician burnout3, The top three contributors are:
- Increasing work hours – On average US physicians spend 51 hrs/week at work and 25% of US physicians spend as much as 60 hrs/week at work3. This has negative implications on work life balance and leads to job dissatisfaction and burnout.
- Increased administrative bureaucratic tasks– these include confusing, misaligned and burdensome regulatory tasks3. These tasks rob US physicians of quality time during the work week that could be spent attending to their patients clinically. In fact for every 1 hour of clinical time a physician spends with their patient there are 2 hrs gained in bureaucratic tasks3. Additionally, US physicians spend over 2 ½ hours per week just completing these tasks3.
- Increased Electronic Medical Related (EMR) related tasks in Practice- Electronic Medical Records (EMRs) and their related tasks3 is another significant contributor to physician burnout. These tasks include clinical chart reviews and completion of documentation, billing and coding, order entry and inbox task completion. Ironically, although EMRs were introduced into healthcare as a tool to help providers streamline workflow and reduce their clerical tasks, it has been shown that physicians have become increasingly burdened by EMRs. Primary care providers spend more than half of an 11.4 hr workday on EMR related tasks with 1.5 hrs of their day spent at home after clinic, oftentimes labeled as “pajama time”3. Therefore, physicians are essentially spending more of their time during their workday completing EMR related tasks rather than direct patient care3.
Impact of Physician Burnout on the Healthcare System
Physician burnout has significant negative implications on the healthcare system. The gravest implication is loss of very talented physicians to suicide. Physician suicide affects female physicians to a greater degree compared to their male colleagues5. The suicide rate among male physicians is 1.41 times higher than the general male population and among female physicians, the relative risk is greater with a 2.27 times greater risk than the general female population5.
Burnout among physicians has negative consequences for patients with association with increased occurrence of major medical errors which also includes burnout among surgeons with a positive correlation of degree of burnout with increased rate of medical errors3.
At an institutional level increasing rates of physician burnout not only leads to increased job dissatisfaction among physicians and high staff turnover rate with loss of very talented physicians but also has negative consequences with decrease in patient satisfaction scores3. This increased staff turnover rate and decreased patient satisfaction scores could potentially lead to loss of revenue due to loss of productivity due to decrease in physician staff and also due to loss of business with patients seeking medical care elsewhere.
Avoiding Physician Burnout
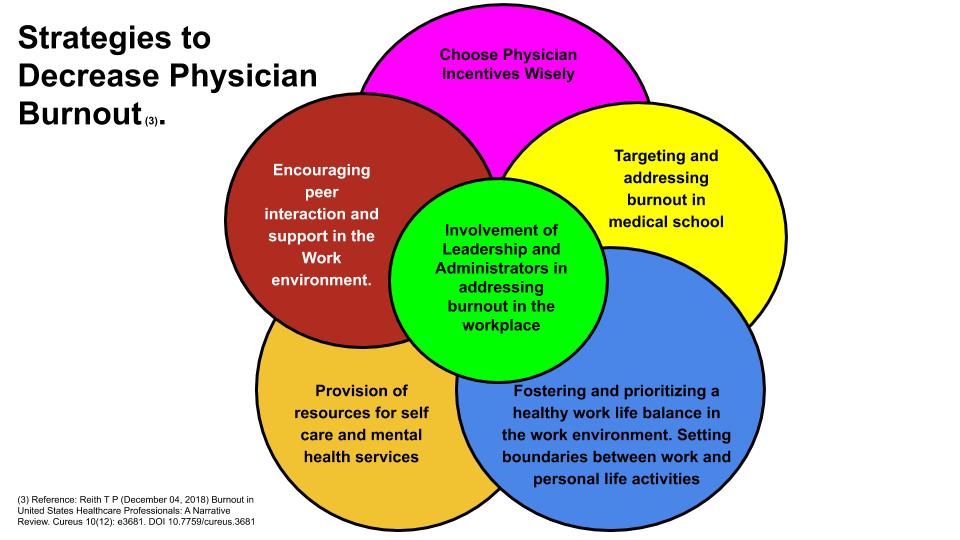
There are several initiatives that have been proposed to decrease physician burnout rates. These initiatives include involvement of leadership and administrators to combat this problem3. A few institutions have included a Chief Wellness Officer whose focus is to improve job satisfaction among physician staff through promoting and fostering an environment that supports physician wellness. It is vital that leadership recognizes burnout as a true problem and prioritize addressing this issue proactively from the top leadership of an institution. This is a key component of combating this problem.
Another initiative to combat burnout is choosing physician incentives wisely3. Many incentives that are chosen by hospitals focus on increased salary through increased productivity based on relative value units (RVU). This often leads to greater physician demands with regards to greater work hours which leads to burnout. However, choosing incentives that are quality based rather than productivity based may have better consequences not only on positively impacting patient care but also reduced physician demands with regards to work hours.
A work environment that fosters and prioritize a healthy work life balance is also important to combat burnout3. This prioritization of work life balance includes an allowance for flexible work schedules. It has been shown that physicians who are able to spend at least 20% of their time on the part of work they find most fulfilling significantly lower their chances of burning out3. In addition, helping physicians to improve their time management may also improve work life balance.
Setting boundaries between work and personal life activities is vital to maintaining a healthy and happy work life balance. Taking work home or completing EMR related tasks at home erodes this balance and should be minimized and ideally avoided. Finding and pursuing hobbies not related to work is also another great way to minimize stress and burnout as well and this should be encouraged in the work environment.
Institutions should also consider providing resources for self care and mental health services to combat burnout3. Physicians could be provided with protected time to seek mental health care confidentially to assist physicians who may have depression or anxiety that requires mental healthcare, Self care tools that could be provided include healthy meal options for physicians in the cafeteria, on site gyms for physicians or providing discounts at local gyms to encourage and promote exercise and self care.
An environment that encourages peer interaction and support can also assist in combating burnout3. Many institutions no longer have physician lounges which was an area where physicians could congregate and discuss the work day and foster a sense of camaraderie3. This is unfortunate as this often leads to reduced social interactions with physician peers and leads to a greater sense of isolation. Institutions should consider providing physician lounges. However, even a small coffee/tea and snack station strategically placed in areas where physicians tend to gather can go a long way to promote social interaction among physicians to build a sense of community. This area has been studied and it has been shown that encouraging physician solidarity reduces burnout and that when physicians are engaged in small group discussions every other week they experienced significant reductions in depersonalization and emotional exhaustion3. Some institutions such as Stanford have found creative ways to promote physician social interaction such as paying for small group physician dinners at local restaurants throughout the work year3.
Targeting and addressing burnout in medical school is vital and has far reaching positive implications as medical students are given or taught the tools necessary to minimize stress, anxiety and depression early in their career. Some medical schools have even revised their curriculum to make it more medical student friendly to decrease stress and burnout and this has been accomplished without sacrificing academic performance3.
Conclusion
Physician burnout remains an increasingly relevant issue within the medical community. There has been a heightening of the awareness of this problem and an attempt in addressing this issue. Although it has been shown that there has been some improvement in work life integration among physicians4, physicians remain at increased risk for burnout compared to individuals in other fields4. It is therefore important that the medical community continue to shine the light on this issue to raise awareness of this problem. It is also important for institutions and medical societies to focus on physician wellness to combat the issue of physician burnout. Happy and fulfilled doctors will most likely result in happy and engaged patients and improved patient care.
References:
- Center, C., Davis, M., Detre, T., Ford, D. E., Hansbrough, W., Hendin, H., Laszlo, J., Litts, D.A., Mann, J., Mansky, P.A., Michels, R., Miles, S.H., Proujansky, R., Reynolds, C.F. 3rd, Silverman, M. M. (2003). Confronting Depression and Suicide in Physicians. JAMA, 289(23), 3161. doi:10.1001/jama.289.23.3161
- Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014 [published correction appears in Mayo Clin Proc. 2016;91(2):276]. Mayo Clin Proc. 2015;90(12):1600-1613.
- Reith T P (December 04, 2018) Burnout in United States Healthcare Professionals: A Narrative Review. Cureus 10(12): e3681. DOI 10.7759/cureus.3681
- Shanafelt TD, West CP, Sinsky C, Trockel M, Tutty M, Satele DV, Carlasare LE, Dyrbye LN. Changes in Burnout and Satisfaction With Work-Life Integration in Physicians and the General US Working Population Between 2011 and 2017. Mayo Clin Proc. 2019 Feb 13. pii: S0025-6196(18)30938-8. doi: 10.1016/j.mayocp.2018.10.023. [Epub ahead of print]
- Schernhammer, E. S., & Colditz, G. A. (2004). Suicide Rates Among Physicians: A Quantitative and Gender Assessment (Meta-Analysis). American Journal of Psychiatry AJP, 161(12), 2295-2302. doi:10.1176/appi.ajp.161.12.2295