The most anticipated cardiovascular conference of the year, AHA Scientific Sessions 2021 is upon us! In the days and hours leading upto the event, speakers have been revising their presentations, moderators going over their notes, and organizers working hard to prevent any glitches for this fully virtual experience. For many attendees, including myself, the most exciting part of the conference is the release of new trial data that may have a bearing on clinical practice and set the direction for future research. This year’s program is heavily ‘charged’ with incredible science in the field of cardiac electrophysiology. Below is a short guide to the studies from the field of electrophysiology being presented in the late breaking science (LBS) sessions.
CRAVE Trial- The Coffee and Real-time Atrial and Ventricular Ectopy (CRAVE) Trial
Presented by Gregory Marcus, MD
LBS.03 Prevention to Intervention in Atrial Arrhythmias, Sunday Nov 14th 8-9 AM EST
Many people report experiencing palpitations with higher caffeine intake and cutting down on coffee is a common advice heard in EP clinics. However, this anecdotal link is not backed by evidence with large population studies showing no association between caffeine intake and arrhythmias.1 Hence, the investigators of the CRAVE trial set out to investigate the effect of caffeine intake on cardiac ectopy.2 Based in University of California, San Francisco, this N-of-1 trial enrolled healthy volunteers and assigned them to 2-day blocks of coffee on-and-off days for 2 weeks. Continuous heart monitors were used to assess the primary outcome i.e., premature atrial and ventricular contractions. The results of this study will be interesting and may finally provide an answer to the important question- to bean or not to bean?
GIRAF Trial- Dabigatran Versus Warfarin on Cognitive Outcomes in Nonvalvular Atrial Fibrillation: Results of the GIRAF Trial
Presented by Bruno Caramelli, MD
LBS.03 Prevention to Intervention in Atrial Arrhythmias, Sunday Nov 14th 8-9 AM EST
Prevention of stroke is one of the pillars of management of atrial fibrillation (AF). However, even in the absence of stroke, patients with underlying AF have an increased risk of cognitive decline and dementia.3 Direct oral anticoagulants (DOACs) such as dabigatran have less food and drug interactions and better safety profiles compared to warfarin and are now considered the preferred agents for long-term stroke prevention in non-valvular AF. However, whether this consistent and stable anticoagulant effect offered by DOACs compared to warfarin translates into prevention or progression of dementia in the elderly patient with AF remains unknown. Investigators of the GIRAF trial conducted a prospective randomized controlled trial (N=200) comparing the effects of dabitran with warfarin on cognitive and functional outcomes at 2 years in an elderly population with AF.4 Clinicians from different fields will be craning their necks for the results of this important trial.
PALACS- Posterior Left Pericardiotomy Reduces Postoperative Atrial Fibrillation After Cardiac Surgery
Presented by Mario F Gaudino, MD
LBS.03 Prevention to Intervention in Atrial Arrhythmias, Sunday Nov 14th 8-9 AM EST
Post-operative AF plagues one-third of patients after cardiac surgery and is associated with longer hospital stays, increased risk of stroke, and higher mortality.5 Drainage of the pericardial cavity into the left pleural place by performing a posterior pericardiotomy has shown benefit in preventing post-operative AF in small studies. In the PALACS study, Dr. Gaudino and colleagues aimed to further assess the impact of posterior pericardiotomy during cardiac surgery on occurrence of post-operative AF.6 If this study also demonstrates a benefit with posterior pericardiotomy, the case for performing this relatively simple surgical procedure will be strengthened.
aMAZE Trial- Outcomes of Adjunctive Left Atrial Appendage Ligation Utilizing the LARIAT Compared to Pulmonary Vein Antral Isolation Alone: The aMAZE Trial
Presented by David Wilber, MD
LBS.03 Prevention to Intervention in Atrial Arrhythmias, Sunday Nov 14th 8-9 AM EST
Persistent symptomatic AF resistant to catheter ablation is an old nemesis of many cardiac electrophysiologists. Pulmonary vein antral isolation (PVI) has a lower success rate in maintaining sinus rhythm for persistent AF as compared with paroxysmal AF. In addition to harboring thrombi, the left atrial appendage (LAA) has been implicated in the maintenance of AF. The surgical Cox-Maze procedure, involving exclusion of the LAA and elimination of foci from in and around the LAA, has shown good results. The aMAZE trial is a randomized open-label trial that evaluated the safety and effectiveness of the transcatheter LARIAT System as an adjunct to PVI in patients with symptomatic persistent and long-standing persistent AF.7 The primary endpoint studied was freedom from episodes of AF > 30 seconds at 12 months. The results of this trial will provide further insight into the utility of LARIAT device LAA occlusion in conjunction with PVI.
I-STOP-Afib Trial- Testing Individualized Triggers of Atrial Fibrillation: A Randomized Controlled Trial
Presented by Gregory Marcus, MD
LBS.04 Information Overload? Striving to Improve Care Delivery Through Digital Health and Automated Data, Sunday Nov 14th 2.45-3.45 PM EST
A group of researchers at University of California, San Francisco have been working to study the triggers of AF in partnership with patients through the Health eHeart Study and StopAfib.org. In preparation for the I-STOP-Afib trial, they conducted a survey of 1,295 patients and found that almost three-quarters of patients self-identified triggers for episodes of AF, most commonly alcohol, caffeine, exercise, and sleep deprivation.8 The I-STOP-Afib study randomized patients to either trials of exposure and elimination of self-identified AF triggers for 6 weeks or symptom surveillance only.9 They used a smartphone application to direct the 2 groups, record daily AF episodes, and assess daily the quality of life at the end of 10 weeks. Regardless of the results, this study will set an example of using technology to empower patients to take charge of their own health.
Detection of Atrial Fibrillation in a Large Population Using Wearable Devices: The Fitbit Heart Study
Presented by Steven Lubitz, MD
LBS.04 Information Overload? Striving to Improve Care Delivery Through Digital Health and Automated Data, Sunday Nov 14th 2.45-3.45 PM EST
Over the past few years, wearable tech has been making waves in the field of EP. Smartwatch based continuous rhythm monitoring has shown promise in the detection of undiagnosed AF. The Fitbit Heart Study is a remote single-arm trial of 450,000 Fitbit device users in the US.10 It is designed to study the validity of a novel software algorithm for detecting AF. The study used compatible Fitbit devices using pulse photoplethysmography to detect irregular heart rhythms and followed abnormal readings with a week-long ECG patch. The strength of the Fitbit Heart Study over prior studies like the Apple Heart Study will be a large, predominantly female population using both iOS and Android smartphone platforms.
Log into AHA Scientific Sessions to livestream the release of these and other exciting trials. Keep buzzing #EPEEPS!
References:
- Voskoboinik A, Kalman JM, Kistler PM. Caffeine and Arrhythmias: Time to Grind the Data. JACC Clin Electrophysiol. 2018;4(4):425-432. doi:10.1016/j.jacep.2018.01.012
- https://clinicaltrials.gov/ct2/show/record/NCT03671759?view=record
- Santangeli P, Di Biase L, Bai R, et al. Atrial fibrillation and the risk of incident dementia: a meta-analysis. Heart Rhythm. 2012;9(11):1761-1768. doi:10.1016/j.hrthm.2012.07.026
- https://clinicaltrials.gov/ct2/show/NCT01994265
- Greenberg JW, Lancaster TS, Schuessler RB, Melby SJ. Postoperative atrial fibrillation following cardiac surgery: a persistent complication. Eur J Cardio-Thorac Surg Off J Eur Assoc Cardio-Thorac Surg. 2017;52(4):665-672. doi:10.1093/ejcts/ezx039
- Abouarab AA, Leonard JR, Ohmes LB, et al. Posterior Left pericardiotomy for the prevention of postoperative Atrial fibrillation after Cardiac Surgery (PALACS): study protocol for a randomized controlled trial. Trials. 2017;18(1):593. doi:10.1186/s13063-017-2334-4
- Lee RJ, Lakkireddy D, Mittal S, et al. Percutaneous alternative to the Maze procedure for the treatment of persistent or long-standing persistent atrial fibrillation (aMAZE trial): Rationale and design. Am Heart J. 2015;170(6):1184-1194. doi:10.1016/j.ahj.2015.09.019
- Groh CA, Faulkner M, Getabecha S, et al. Patient-reported triggers of paroxysmal atrial fibrillation. Heart Rhythm. 2019;16(7):996-1002. doi:10.1016/j.hrthm.2019.01.027
- https://clinicaltrials.gov/ct2/show/study/NCT03323099
- Lubitz SA, Faranesh AZ, Atlas SJ, et al. Rationale and design of a large population study to validate software for the assessment of atrial fibrillation from data acquired by a consumer tracker or smartwatch: The Fitbit heart study. Am Heart J. 2021;238:16-26. doi:10.1016/j.ahj.2021.04.003
“The views, opinions and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your personal health matters. If you think you are having a heart attack, stroke or another emergency, please call 911 immediately.”

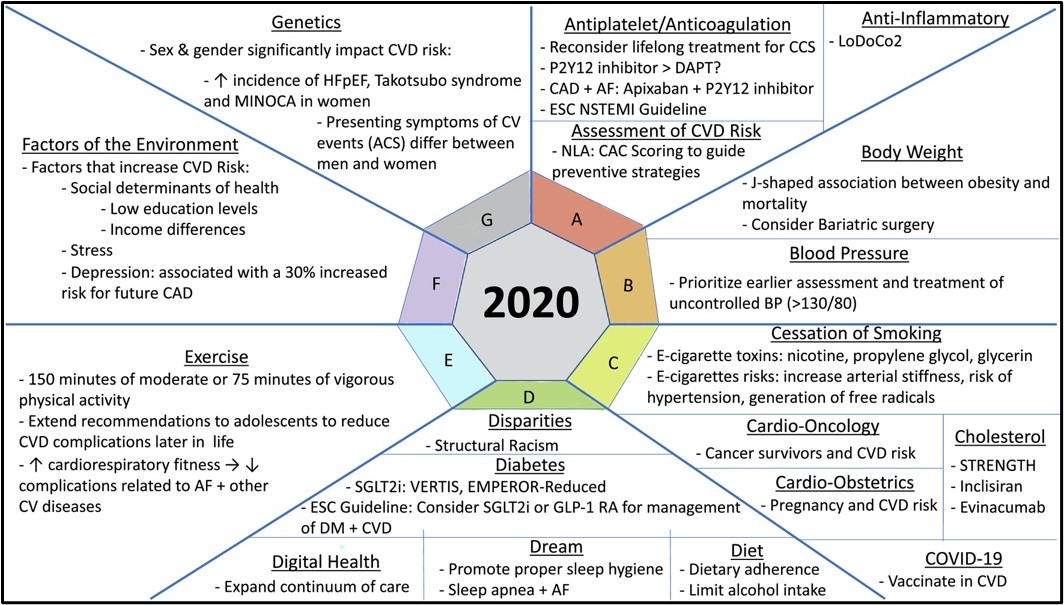 To improve quality of life in ageing population, other symptoms of ageing including physiological function decline start to capture scientific community’s attention. In AHA Scientific Sessions 2021, a panel of experts and professionals in the field talked about novel strategies to promote healthy vascular aging.
To improve quality of life in ageing population, other symptoms of ageing including physiological function decline start to capture scientific community’s attention. In AHA Scientific Sessions 2021, a panel of experts and professionals in the field talked about novel strategies to promote healthy vascular aging.