“Led by a new paradigm, scientists adopt new instruments and look in new places” – Thomas S. Kuhn
For a lot of rational (and some irrational) reasons, hearing the word HIV evokes fear, anger, and sadness. When I first heard about HIV, I was an elementary school student in late 1980’s and at that time, HIV was almost always a death sentence. But today that is not the case. Today, due to the hard work of scientists, patients, volunteers, advocates, and countless others, HIV is a chronic, manageable disease. An accomplishment epitomized by the oldest known person living with HIV recently turning 100 years old.
While this progress and longevity should be celebrated, the flip-side of age is that it is the primary driver of cardiovascular disease (CVD). In fact, this longevity has ushered in a new era where adults living with HIV are at exceptionally high risk of cardiovascular diseases including heart attacks, heart failure, and stroke. A recent meta-analysis by Anoop Shah, MD, from the University of Edinburgh, found that the global burden of HIV-associated cardiovascular disease has tripled in the past 20 years, especially in low and middle-income countries. Now, after more than two decades of accumulating evidence in this field, the American Heart Association released earlier this month a Scientific Statement on the characteristics, prevention and management of cardiovascular disease in people living with HIV.
Directed at all who support adults living with HIV, this statement is a general roadmap for raising awareness about the increasing burden of CVD in this population. However, it offers few new tools for providers to use, due primarily to the lack of high-quality “clinical trial data on how to prevent and treat cardiovascular diseases in people living [and aging] with HIV investigating cardiovascular endpoints” said Matthew J. Feinstein, M.D., M.Sc., chair of the writing group for the statement and assistant professor of medicine at the Feinberg School of Medicine, Northwestern University.
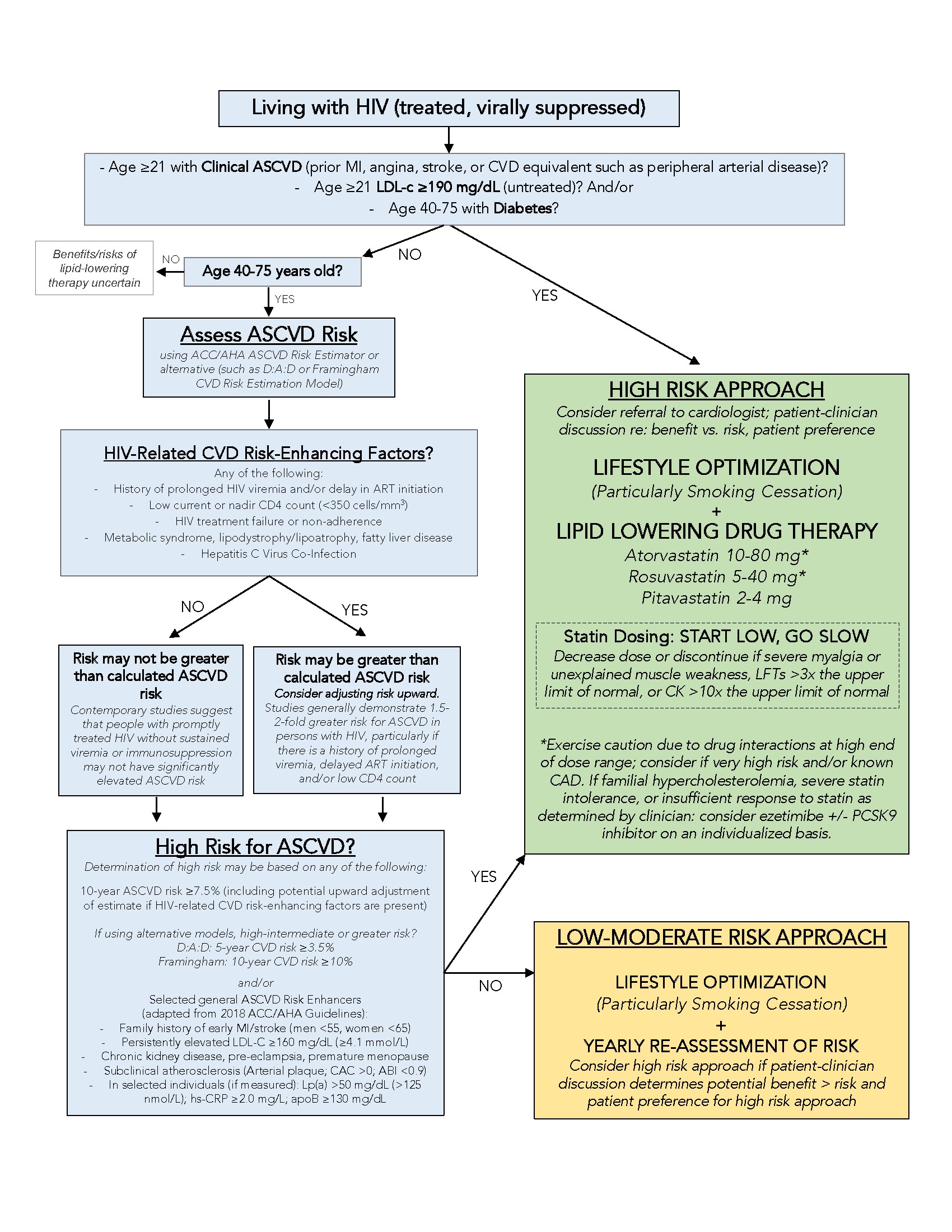
Still, what the existing (mostly observational) evidence allowed the writing group to do was to develop a pragmatic approach to assessing and preventing cardiovascular disease in treated HIV (Figure above). This approach includes the following:
- Ensure all patients living with HIV are on effective HIV treatment
- Determine risk of cardiovascular disease using tools such as ACC/AHA 10-year ASCVD risk estimator and a family history
- Optimize lifestyle approach to prevention (e.g., smoking cessation, physical activity, healthy diet intake)
- If at high risk and between the ages of 40-75 years, talk with the patient about the risks and benefits of lipid-lowering therapy while exercising caution for drug-drug interactions
Yet, while the new AHA Scientific Statement will be an important catalyst for the field, in many ways it creates more questions than answers. For example, are we shifting to a new paradigm in HIV care? Do we need new tools to help reduce CVD in this population or are the general recommendations for risk stratification and lifestyle optimization sufficient? What is the most effective way to get either existing or new clinical tools to the high-risk patients living with HIV?
Fortunately, some of these questions are starting to be answered. The REPRIEVE study is the first large scale (>8,000 people) clinical trial to test if a daily statin reduces cardiovascular disease in adults living with HIV. Results are expected in the next 3-4 years. Additionally, the PRECluDe grants at the National Heart, Lung, and Blood Institute have stimulated new implementation science research focused on understanding how to best adapt effective CVD prevention studies to the real-world settings where people living with HIV receive their health care. These initiatives, coupled with ongoing research on the discovery of mechanisms of CVD and the testing of CVD prevention interventions in people living with HIV, will eventually allow for the development of guidelines on the prevention and management of CVD in HIV—the true instrument needed to help improve cardiovascular health for all adults living with HIV.