As the population continues to age, along with the addition of lifesaving and prolonging medical therapies, the prevalence of HF will continue to increase. In this article, we will solely focus on Heart Failure with Reduced Ejection Fraction (HFrEF), and the potential solutions to the issues with the optimization of guideline directed medical therapy (GDMT) on a systems level.
Robust evidence has established a mortality benefit of GDMT for patients with left ventricular dysfunction. Although the known benefits of GDMT have continued to solidify, there remains a visible gap among patients with HFrEF and the efficacy of treatment.
The issues that exist are likely not based on the individual pharmaceutical therapies profile. Furthermore, medication intolerance and incomplete prescription data can only partially be blamed. Nevertheless, the problems are on a bigger scale, and they involve many different components of our care system.
Let’s discuss some of the barriers to the optimization of GDMT in patients with HFrEF: patient providers and the care system. Providers, including non-cardiologists, should be trained adequately to be able to initiate patients on appropriate medications for HFrEF. They should also know the threshold to discontinue the medications, their side effects, the major contraindications, and, most importantly, when to seek help. HF patients are often complex, and it is essential to know that the different providers involved in their care should be in constant communication when it comes to their medical regimen. It is not enough to start the medication. It’s of utmost importance to continue increasing the dosages as tolerated by the patient to at least the dosages used in the different studies where these medications have shown the most benefits. Education is a key aspect, and it should involve the patient, patient’s family, providers, and everybody in the care system responsible for the patient including nurses and pharmacists. I propose 2 points among many out there:
- Standardized education for everybody involved in the patient’s care
- Standardized methods of communication between the different providers involved in the patient’s care including the patient and their families.
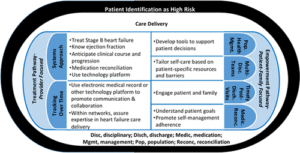
Figure 1. Heart Failure Summit 2017 Overview: Improving care and outcomes in heart failure1.
The purpose of this article is not to re-invent the wheel. The American Heart Association Heart Failure Summit in 2017 identified opportunities to improve care and outcomes and reduce disparities for patients with HF.(Figure 1). The purpose of this article is to remind us that we should be focusing more on implementation strategies for GDMT. We already have the tools, and, as we speak, we are adding new ones. It’s not just the tools; it is how you make use of them that will be the difference.
In summary, establishing and implementing systems of care that can help increase the number of patients on GDMT with the focus on improving medication adherence will ultimately lead to better outcomes. What is certain is that we must continue to meet the challenges of the realities of GDMT and their barriers. Our patients with heart failure depend on it.
References
- Pamela N. Peterson. Circulation: Heart Failure. The American Heart Association Heart Failure Summit, Bethesda, April 12, 2017, Volume: 11, Issue: 10, DOI: (10.1161/CIRCHEARTFAILURE.118.004957)
The views, opinions and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your personal health matters. If you think you are having a heart attack, stroke or another emergency, please call 911 immediately.