Cardiovascular diseases (CVD) are the leading cause of death in Western countries and accounts for 17.3 million deaths/year globally1. In the United States, one in every three deaths are caused by CVD, and more than 130 million adults are projected to express CVD by 2035 clinically1. The unhealthy diet and physical inactivity, obesity, stress, smoking, and alcohol consumption are major risk factors for CVD development1. Nutrition has been reported to be the most preventable risk factor of CVD death1,2. Further, a healthy diet is crucial for managing body weight, diabetes, and hypertension1,3. Therefore, it is essential to identify foods and dietary patterns beneficial for cardiovascular health.
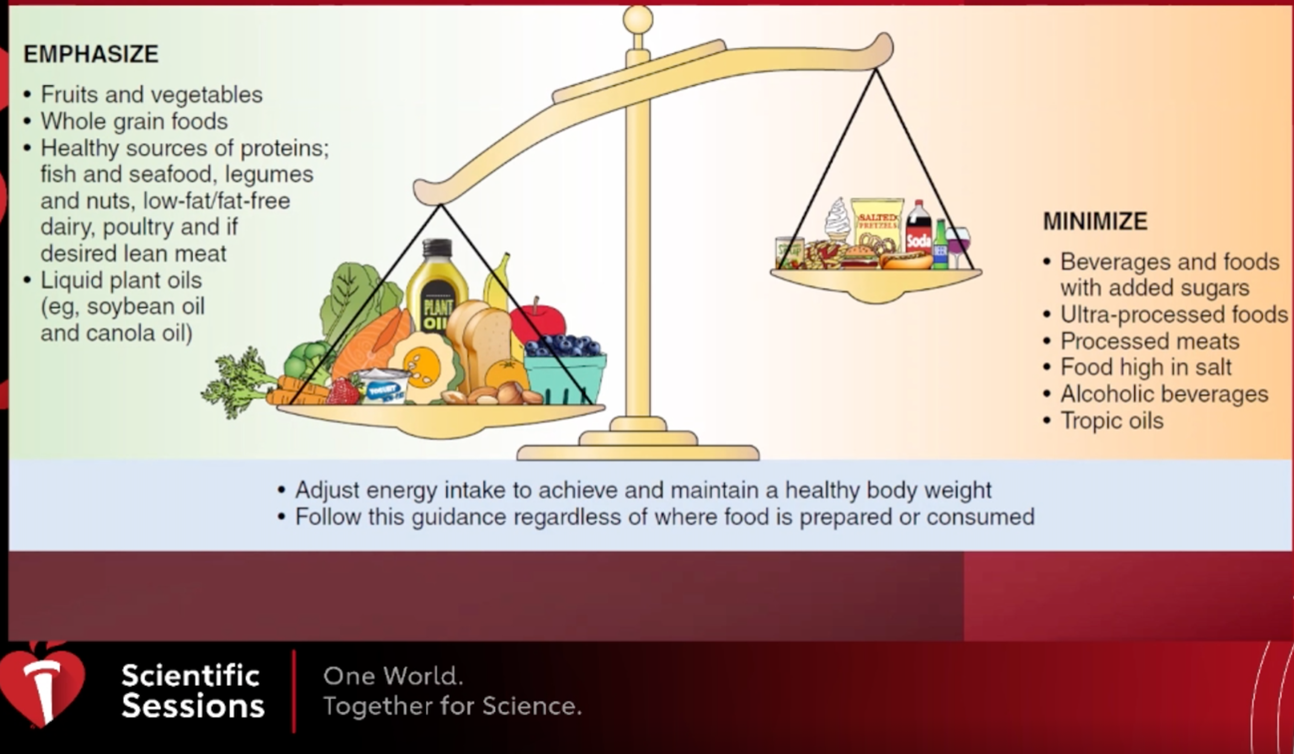
AHA 2021 Dietary Guidance to Improve Cardiovascular Health was presented for the first time by Dr. Alice Lichtenstein, a lead scientist at Tufts University, at #AHA21 scientific sessions and was recently published in Circulation4. AHA suggests that instead of emphasizing one food/nutrient, one should focus on dietary patterns that are the sum of all foods and beverages consumed4. The dietary habits can be adapted to personal preferences, ethical/religious practices, and life stages so that healthy patterns can be followed in the long run4. A heart-healthy diet promotes a healthy planet, meets essential nutrients and fiber requirements, and benefits stroke, type 2 diabetes, kidney disease, and cognitive function4. AHA 2021 Dietary Guidance is organized in following ten features:
- Adjust energy balance to achieve and maintain healthy body weight.
- Include plenty and a variety of fruits and vegetables.
- Pick food made with whole grains rather than refined grains.
- Choose healthy protein sources, mostly plants, fish, and seafood, and low-fat/fat-free dairy products. If meat or poultry is desired, replace red and processed meat with lean cuts and unprocessed form.
- Use liquid plant oils rather than tropical oils and trans-fat.
- Choose minimally processed foods.
- Minimize consumption of beverages and foods with added sugars.
- Consume food prepared with no or little salt.
- Limit intake of alcohol. If you do not drink alcohol, do not start.
- Adhere to this guidance regardless of where food is prepared or consumed,
However, is it easy for everyone to follow a heart-healthy diet? Our food environment is an essential element when we talk about diet quality and can make it difficult for people to adhere to heart health guidelines. Although diet quality improved from 1999 to 2012, disparities are evident based on race/ ethnicity, education, and income5. Dr. Maya Vadiveloo, assistant professor at the University of Rhode Island, explained that the food environment mainly consists of:
- Regulatory environment (federal, state, and local practices, and food marketing).
- Physical environment (places we eat, live, and acquire food).
- Social environment (family and peers).
- Individual choices.
She further explained that several state and federal policies, structural racism, neighborhood segregation, unhealthy built environments impede the adaption to a healthy diet. Furthermore, availability, price, and varied access make choosing unhealthy and processed food easier4. Federal food assistance programs, including Supplemental Nutrition Assistance Program (SNAP) and the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), are not universally effective and only cover a fraction of the monthly household supply4. Food companies tend to target low-income and racial minorities households. High processed food and beverages are telecasted more on TV, digital media, and print advertisements4. Dr. Vadiveloo concluded her talk by discussing the concept of precision nutrition which includes the evaluation of genetics, microbiome, dietary intake, and socioeconomic and physical environment to determine the most fruitful dietary plan to prevent and treat disease. Increased access to affordable housing, enhancing access to supermarkets and green space, and increased access to online food delivery can help achieve dietary goals. She emphasized the power of artificial intelligence, which is unfortunately used for promoting unhealthy food. Still, it can help design personalized dietary interventions, population-level diet quality, and help people choose healthier and medical tailored diets when they buy groceries.
Following this, Dr. Lawrence J Appel, professor at John Hopkins University, explained how a multisector approach including government (regulatory and agriculture policy), health care sector, private sector, and health advocacy organizations is needed to change the default of food sector/eating. Dr. Appel focused on how policy changes can help individuals to eat healthily. In the US, processed and restaurant foods are significant sources (>70%) of sodium6. FDA generated guidance for food manufacturers and restaurants to reduce salt in their processed, packaged, and prepared foods to achieve a 12% reduction in sodium and slash rates of heart diseases7. WHO has generated public food procurement policies that require food and beverages served/sold in a public setting to promote a healthy diet8, indirectly influencing manufacturers to reformulate their products. Although not common in the US, several other countries have front-of-pack warning labels (nutrient specific labels, nurtiscore and guideline daily amount) and health taxes on sugary drinks and salty food. Currently, only New York City requires restaurants to post a warning label next to the menu that contains more than 2300 mg of sodium and applies to restaurants with more than 15 locations nationwide. He concluded his talk by the importance of advocating and supporting policies that improve the health of patients and the broader community.
The last talk of the session was by Dr. Anne N. Thorndike from Massachusetts General Hospital and Harvard Medical school. Dr. Thorndile explained how clinicians and the healthcare sector could help implement 2021 dietary guidelines. She suggested that clinicians emphasize overall nutritional patterns and ask patients about barriers to access and consuming a healthy diet. Further, a clinician can deliver simple patient-centered guidance consistently over time by encouraging fruits/vegetables, plant proteins and oils, whole grains and discouraging the use of added sugars, processed meat, and excess alcohol. Further, hospitals employ approximately 6 million people and treat 750 million people annually. Therefore, many patients are exposed to cafeteria food. Hospitals can opt for traffic-light labels to promote healthy eating where green light suggests choosing often, yellow light means choosing less often, and a red light indicates a better choice available.
There is plethora of scientific evidence present that have helped in building 2021 AHA dietary guidelines. However, we need a multisector approach which will help imply the dietary goals to a larger population.
Reference
- Casas R, Castro-Barquero S, Estruch R, Sacanella E. Nutrition and Cardiovascular Health. Int J Mol Sci. Dec 11 2018;19(12)doi:10.3390/ijms19123988
- Mozaffarian D, Ludwig DS. Dietary guidelines in the 21st century–a time for food. JAMA. Aug 11 2010;304(6):681-2. doi:10.1001/jama.2010.1116
- Lacroix S, Cantin J, Nigam A. Contemporary issues regarding nutrition in cardiovascular rehabilitation. Ann Phys Rehabil Med. Jan 2017;60(1):36-42. doi:10.1016/j.rehab.2016.07.262
- Lichtenstein AH, Appel LJ, Vadiveloo M, et al. 2021 Dietary Guidance to Improve Cardiovascular Health: A Scientific Statement From the American Heart Association. Circulation. Dec 07 2021;144(23):e472-e487. doi:10.1161/CIR.0000000000001031
- Rehm CD, Peñalvo JL, Afshin A, Mozaffarian D. Dietary Intake Among US Adults, 1999-2012. JAMA. Jun 21 2016;315(23):2542-53. doi:10.1001/jama.2016.7491
- Harnack LJ, Cogswell ME, Shikany JM, et al. Sources of Sodium in US Adults From 3 Geographic Regions. Circulation. May 09 2017;135(19):1775-1783. doi:10.1161/CIRCULATIONAHA.116.024446
- Edward E. New FDA guidance aims to drastically cut salt in food supply. NBC News. Accessed December 15, 2021. https://www.cnbc.com/2021/10/13/new-fda-guidance-aims-to-drastically-cut-salt-in-food-supply.html
- Public Food Procurement and Service Policies for Healthy Diet. WHO. Accessed December 15, 2021. https://apps.who.int/iris/bitstream/handle/10665/338525/9789240018341-eng.pdf
“The views, opinions and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your personal health matters. If you think you are having a heart attack, stroke or another emergency, please call 911 immediately.”