Atherosclerotic cardiovascular disease (CVD) prevention has been traditionally divided into primary or pre-event prevention and secondary or re-event prevention. The AHA 2021 joint session with the American Society of Preventive Cardiology entitled “Blurred Lines-Overlap in High-Risk Primary Prevention vs Secondary Prevention” challenged this traditional concept. The session tackled the case of a high-risk patient where using stricter treatment approaches, usually applied in secondary prevention, might be more relevant for her primary prevention. The invited speakers gave an overview of the different treatment options currently available for high-risk primary prevention and highlighted the knowledge gaps in the field.
It is well established that most cardiovascular events (CVE), such as myocardial infarction (MI) and stroke, occur in patients with prior no symptoms. When it comes to predicting CVE, it has been shown that the plaque burden (calculated by Coronary Artery Calcium (CAC) score for example) is a better predictor than the severity of stenosis. This is because the type and certain features of an atherosclerotic plaque can render it more vulnerable regardless of the stenosis degree.
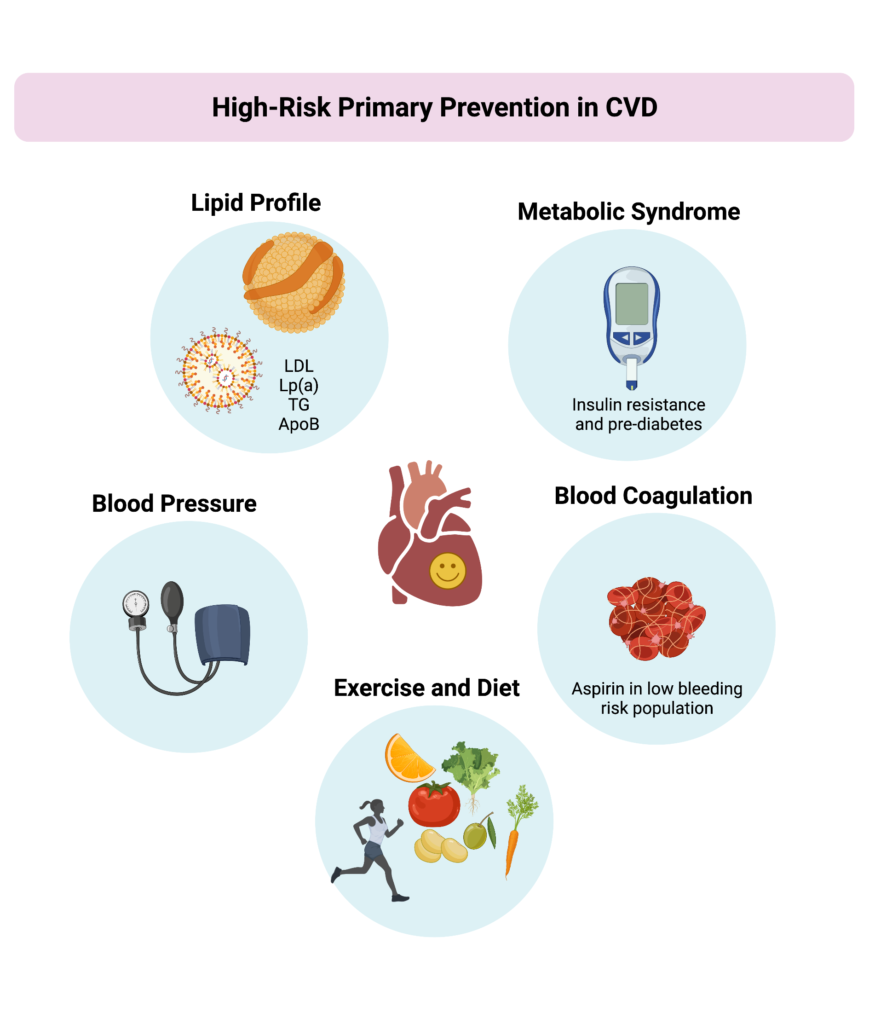
The lines between primary and secondary prevention become blurry when studies such as the one recently conducted by Peng and colleagues demonstrated that primary prevention individuals with very high CAC score (~900) had a similar rate of CVE compared to stable treated high risk secondary prevention patients such as those in the FOURRIER trial. These results show that high-risk primary prevention population might benefit from intense management. Additional risk factors can be taken into account when optimizing the treatment while keeping in mind that not all high-risk primary prevention patients are the same despite presenting with a high CAC score. Before selecting a treatment strategy for a high-risk patient in primary prevention, it is important to evaluate the severity of the patient’s risk factors and act on them accordingly.
Reducing LDL-C levels, ideally below 70 mg/dl, is a good starting point. This can be done using intensive statin therapy or adding ezetimibe or a PCSK9 inhibitor for patients with additional risk factors who do not achieve LDL-C targets. It is of note that PCSK9 inhibitors can reduce Lp(a), triglycerides and ApoB levels which are known to increase CVD risk. The ongoing VESALIUS trial is evaluating the effect of using the PCSK9 inhibitor evolocumab on CVE in primary prevention high-risk patients with no history of myocardial infarction or stroke. For patients with high triglyceride levels, the results of the REDUCE-IT trial demonstrated a reduction of CVE (CV deaths, MI and stroke) when using icosapent ethyl, an EPA derivative. In this trial, 1% of patients had an increase in atrial fibrillation and atrial flutter which can be managed considering the advantageous reduction in stroke risk. However, the REDUCE-IT trial was conducted in a prevalent secondary prevention population and the benefit in high-risk primary prevention needs to be further investigated.
Metabolic syndrome is another risk factor than can be monitored in high-risk primary prevention as it increases the risk of CVE and type 2 diabetes. SGTL2 inhibitors have been shown to reduce CVE in patients with heart failure and reduced ejection fraction offering a benefit of using this anti-diabetic drug class in a non-diabetic population. About a third of the patients enrolled in the CANVAS trial were high-risk primary prevention and had a reduction of CVE while using SGLT2 inhibitors. The REWIND trial on the other hand, which enrolled about 69% of high-risk primary prevention patients, showed that GLP1-RA, another class of anti-diabetics, decreased the occurrence of CVE. However, SGLT2 and GLP1-RA are not yet FDA approved for high-risk primary prevention and the current alternative is managing lifestyle. Patients with metabolic syndrome can be advised to improve the quality (Mediterranean and DASH diets) and quantity (1600 to 3000 calories) of their diet and encouraged to include a fasting period of 14 hours per day to improve their blood pressure and atherogenic lipids profile.
In addition to controlling lipids, blood pressure and pre-diabetes, aspirin can also be considered for high-risk patients in primary prevention but only in those with low bleeding risk as shown by the recent data from the Dallas Heart Study (DHS).
References
- Van Venrooij FV, Stolk RP, Banga JD, Erkelens DW, Grobbee DE. Primary and secondary prevention in cardiovascular disease: an old-fashioned concept? J Intern Med. 2002;251(4):301–6.
- Mortensen MB, Dzaye O, Steffensen FH, B øtker HE, Jensen JM, R ønnow SNP, et al. Impact of Plaque Burden Versus Stenosis on Ischemic Events in Patients With Coronary Atherosclerosis. J Am Coll Cardiol. 2020 Dec 15;76(24):2803–13.
- Peng AW, Dardari ZA, Blumenthal RS, Dzaye O, Obisesan OH, Iftekhar Uddin S m., et al. Very High Coronary Artery Calcium (≥1000) and Association With Cardiovascular Disease Events, Non–Cardiovascular Disease Outcomes, and Mortality. Circulation. 2021 Apr 20;143(16):1571–83.
- Arbab-Zadeh A, Fuster V. From Detecting the Vulnerable Plaque to Managing the Vulnerable Patient: JACC State-of-the-Art Review. J Am Coll Cardiol. 2019 Sep 24;74(12):1582–93.
- Amgen. A Double-blind, Randomized, Placebo-controlled, Multicenter Study to Evaluate the Impact of Evolocumab on Major Cardiovascular Events in Patients at High Cardiovascular Risk Without Prior Myocardial Infarction or Stroke [Internet]. clinicaltrials.gov; 2021 Dec [cited 2021 Dec 10]. Report No.: NCT03872401. Available from: https://clinicaltrials.gov/ct2/show/NCT03872401
- McMurray JJV, Solomon SD, Inzucchi SE, Køber L, Kosiborod MN, Martinez FA, et al. Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction. N Engl J Med. 2019 Nov 21;381(21):1995–2008.
- Wilkinson MJ, Manoogian ENC, Zadourian A, Lo H, Fakhouri S, Shoghi A, et al. Ten-Hour Time-Restricted Eating Reduces Weight, Blood Pressure, and Atherogenic Lipids in Patients with Metabolic Syndrome. Cell Metab. 2020 Jan 7;31(1):92-104.e5.
- Bhatt DL, Steg PG, Miller M, Brinton EA, Jacobson TA, Ketchum SB, et al. Cardiovascular Risk Reduction with Icosapent Ethyl for Hypertriglyceridemia. N Engl J Med. 2019 Jan 3;380(1):11–22.
- Ajufo E, Ayers CR, Vigen R, Joshi PH, Rohatgi A, de Lemos JA, et al. Value of Coronary Artery Calcium Scanning in Association With the Net Benefit of Aspirin in Primary Prevention of Atherosclerotic Cardiovascular Disease. JAMA Cardiol. 2021 Feb 1;6(2):179–87.
“The views, opinions and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your personal health matters. If you think you are having a heart attack, stroke or another emergency, please call 911 immediately.”