Climate Change and Cardiovascular Diseases

Climate change is partly due to the increased atmospheric concentration of greenhouse gases emitted by burning fossil fuels like oil, natural gas, and methane produced by ruminant agricultural animals. The earth’s temperature has augmented by 0.85°C in the last century, and the rate of global warming has increased to 0.18°C/decade in the last three decades. The altering temperature, in particular increasing heat, is one of the critical features of climate change and can significantly affect cardiac health. In addition, extreme weather events, rising sea levels, and lack of food and water are expected outcomes of climate change1.
Cardiovascular Diseases (CVDs) are the leading cause of death globally, and climate change can worsen CVD incidence further. Heatwaves are expected to be more frequent and prolonged due to ongoing climate change. The intense heat can cause mortality and morbidity due to heatstroke, which is defined as hyperthermia associated with a systemic inflammatory response resulting in multiple organ failure and predominant encephalopathy. Heat stress is associated with acute cardiac events where heated blood circulates in peripheral circulation, and heat tolerance is impaired due to insufficient cardiac output to meet the body’s needs for sufficient heat loss1.
There is a U-shaped relationship between temperature and all-cause mortality where mortality increases with the shift from ‘optimum temperature’ at both cold and hot ends. In the Netherlands, the lowest mortality rate was observed with an average temperature of 16.5°C, and CVD mortalities accounted for 57% of cold-related death2. In 1976, daily deaths from coronary thrombosis increased two-fold during the London heatwave3. Additionally, daily mortality due to congestive heart failure is strongly associated with maximum daily temperature in Montreal, with an exponential increase starting at 25°C4. Similarly, during comparatively hotter summer, a U-shaped relationship between outer temperature and coronary artery disease deaths is reported in Taiwan5.
Lifestyle modifications on a large population scale are required to reduce the emission of greenhouse gases, thereby mitigating the extent of climate change. Reducing the use of motor vehicles for short-distance commuting can help reduce the emissions of greenhouse gases related to transportation and air pollution that can have adverse effects on health. Further, reducing the consumption of ruminant meat such as sheep and cows and increasing the use of renewable energy, including solar radiation or wind power, can help mitigate climate change, air pollution, and the risks of heart diseases1.
Another essential remedy to diminish climate change can be ‘active transport or self-transport that encompasses more physical activity and involves walking, cycling, and use of public transport as a mode of transportation. This will not only reduce the emanation of greenhouse gases but increased physical activity can confer several cardiac health benefits1. An extra kilometer walk is associated with a 4.8% reduction in risk of obesity which is a significant risk factor of CVD, whereas an extra hour spent in car/day is lined with a 6% increase in the likelihood of obesity6. Additionally, a study done in Finland reported a significant reduction in CVD risk and all-cause mortality in women who walked or cycled 15 minutes or more for work7.
In conclusion, we need to modify our lifestyle and make healthier choices to protect our hearts and earth. If you are further interested in the topic, you can get a detailed insight in the review article published in the Cardiology journal1 titled “The effects of climate change on cardiac health”.
REFERENCE
- De Blois J, Kjellstrom T, Agewall S, Ezekowitz JA, Armstrong PW, Atar D. The Effects of Climate Change on Cardiac Health. Cardiology. 2015;131(4):209-17. doi:10.1159/000398787
- Kunst AE, Looman CW, Mackenbach JP. Outdoor air temperature and mortality in The Netherlands: a time-series analysis. Am J Epidemiol. Feb 01 1993;137(3):331-41. doi:10.1093/oxfordjournals.aje.a116680
- Keatinge WR, Coleshaw SR, Easton JC, Cotter F, Mattock MB, Chelliah R. Increased platelet and red cell counts, blood viscosity, and plasma cholesterol levels during heat stress, and mortality from coronary and cerebral thrombosis. Am J Med. Nov 1986;81(5):795-800. doi:10.1016/0002-9343(86)90348-7
- Kolb S, Radon K, Valois MF, Héguy L, Goldberg MS. The short-term influence of weather on daily mortality in congestive heart failure. Arch Environ Occup Health. 2007;62(4):169-76. doi:10.3200/AEOH.62.4.169-176
- Pan WH, Li LA, Tsai MJ. Temperature extremes and mortality from coronary heart disease and cerebral infarction in elderly Chinese. Lancet. Feb 11 1995;345(8946):353-5. doi:10.1016/s0140-6736(95)90341-0
- Frank LD, Andresen MA, Schmid TL. Obesity relationships with community design, physical activity, and time spent in cars. Am J Prev Med. Aug 2004;27(2):87-96. doi:10.1016/j.amepre.2004.04.011
- Barengo NC, Hu G, Lakka TA, Pekkarinen H, Nissinen A, Tuomilehto J. Low physical activity as a predictor for total and cardiovascular disease mortality in middle-aged men and women in Finland. Eur Heart J. Dec 2004;25(24):2204-11. doi:10.1016/j.ehj.2004.10.009
“The views, opinions, and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness, and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions, or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your health matters. If you think you are having a heart attack, stroke, or another emergency, please call 911 immediately.”
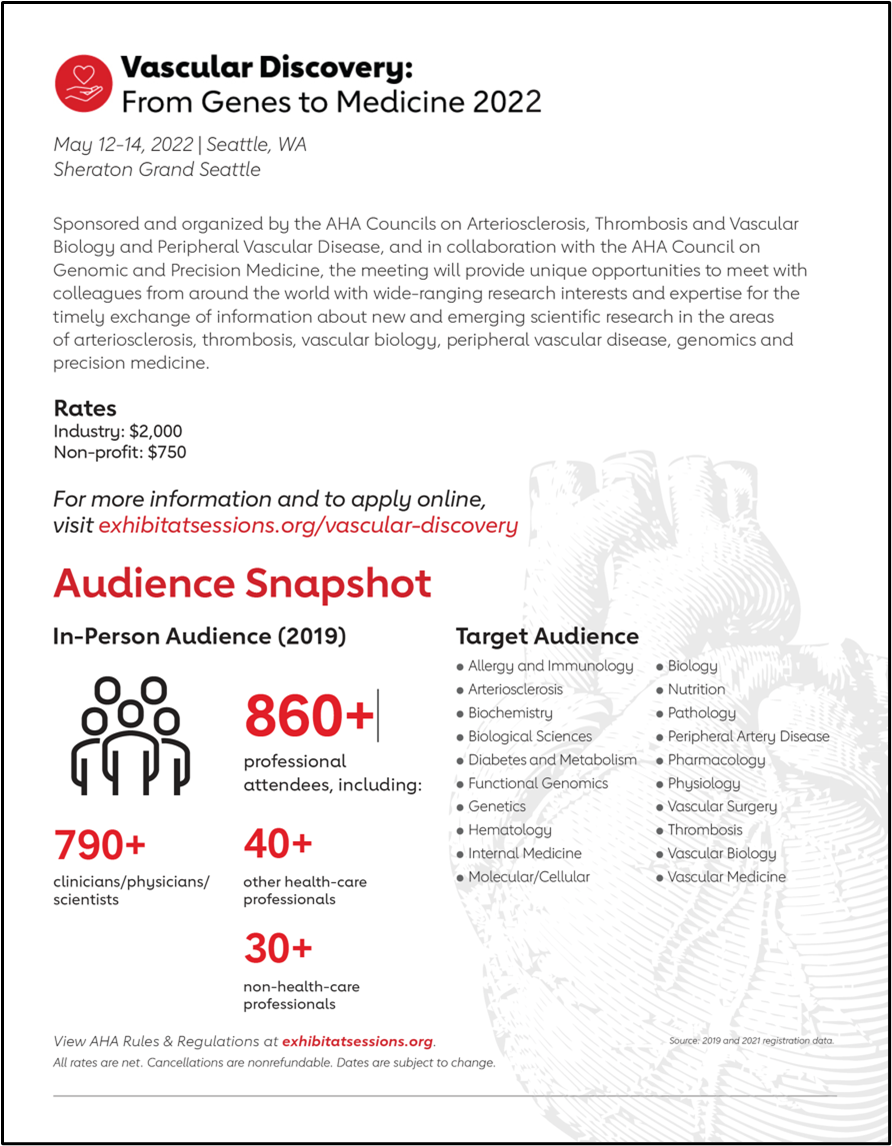 You might want to check out Vascular Discovery 2022, a 2 ½-day meeting, which is sponsored by the Council on Arteriosclerosis, Thrombosis and Vascular Biology, the Peripheral Vascular Disease Council, and the Council on Genomic and Precision Medicine, in cooperation with and the Society for Vascular Surgery’s Vascular Research Initiatives Conference (Flyer on the right).
You might want to check out Vascular Discovery 2022, a 2 ½-day meeting, which is sponsored by the Council on Arteriosclerosis, Thrombosis and Vascular Biology, the Peripheral Vascular Disease Council, and the Council on Genomic and Precision Medicine, in cooperation with and the Society for Vascular Surgery’s Vascular Research Initiatives Conference (Flyer on the right).
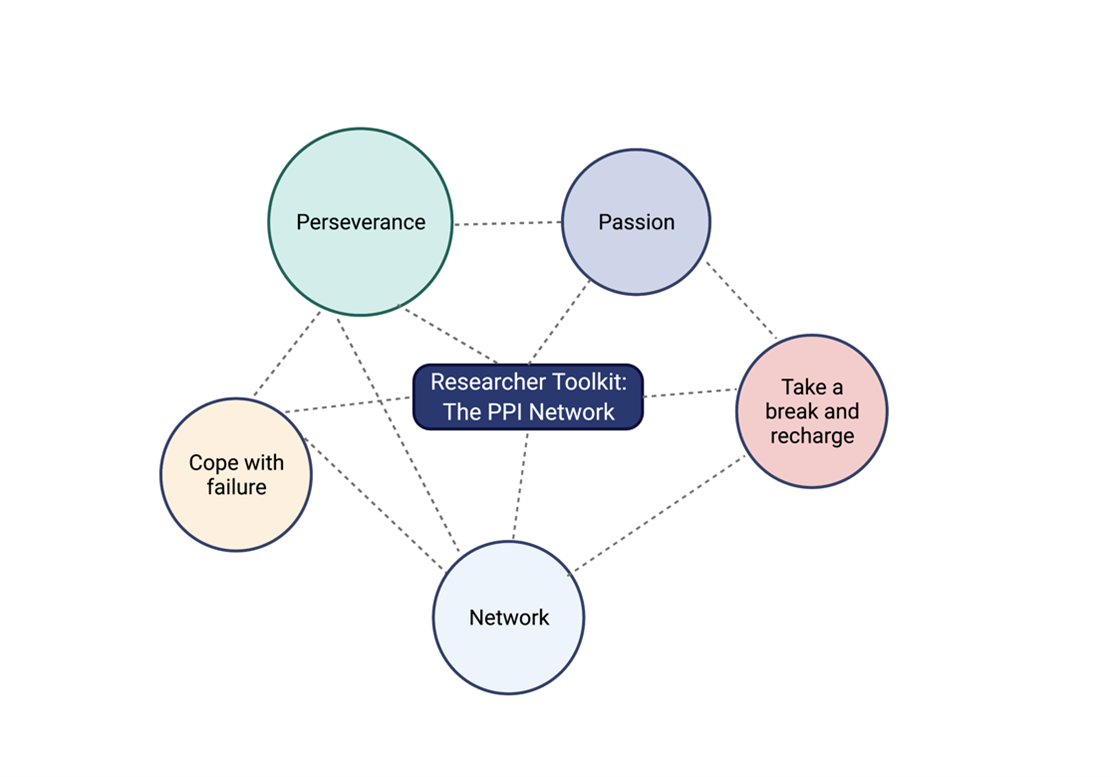
 I had the pleasure of having a one-on-one virtual meet-up with Mabruka Alfaidi MD, PhD who won the ATVB Investigator in Training Award Competition during last year’s Vascular Discovery 2021 meeting based on her fascinating work on endothelial cells and IL-1b signaling pathway as well as her active involvement with the research community. We discussed her career path and her future projects which we couldn’t do without also going over the many hurdles that come our way as researchers. I decided to summarize the main themes that we tackled in a researcher’s toolkit which encompasses key ingredients to sustain a career in research: The PPI network.
I had the pleasure of having a one-on-one virtual meet-up with Mabruka Alfaidi MD, PhD who won the ATVB Investigator in Training Award Competition during last year’s Vascular Discovery 2021 meeting based on her fascinating work on endothelial cells and IL-1b signaling pathway as well as her active involvement with the research community. We discussed her career path and her future projects which we couldn’t do without also going over the many hurdles that come our way as researchers. I decided to summarize the main themes that we tackled in a researcher’s toolkit which encompasses key ingredients to sustain a career in research: The PPI network.