COVID-19 Vaccine: What We Need To Know
While we are living in the third peak of COVID-19 pandemic, we have been delighted to hear about the recent food and drug administration (FDA) approval of the COVID-19 vaccine, after trials involving hundreds or more of patients showed the vaccine safety and efficacy [1,2]. However, the COVID-19 vaccine is associated with some side effects, which in fact might be more common than the flu vaccine. Healthcare workers and first responders will have the priority to get the vaccine at many institutions given their high-risk work environment. So, I decided to share some knowledge about some of the side effects of the vaccine I recently read about and how institutions are planning to stagger the vaccines among their employees.
What are the side effects of the vaccine?
Side effects seem to be more common than the annual flu vaccine, with arm pain at the injection site, generalized fatigue and malaise, headaches, dizziness, fever, chills, nausea, vomiting, and diarrhea. Rare side effects include Bell’s palsy and temporary facial muscle paralysis. Most of these side effects are mild and resolve in a few days. These side effects occur more frequently after the second dose of the vaccine. These side effects actually suggest reactogenicity and that the immune system is responding to the vaccine [1,2].
Are there long-term adverse events of the COVID-19 vaccine?
This is still unknown and under close monitoring by FDA [1].
How will the vaccine change things from now on?
The COVID-19 vaccine is an additional protection layer, but it does not substitute the other protection measures we have been following; that means we should still conform to social distancing and follow hygienic instructions wherever we go till the pandemic is over. This pandemic has taught us all, as a healthcare professional and as members of the community, to be responsible for our actions toward each other and persist despite all the obstacles. The vaccine could be the first step that leads us back to “normal life” as long as we stay responsible for each other.
REFERENCES
[1] Walsh EE, Frenck RW Jr, Falsey AR, et al. Safety and Immunogenicity of Two RNA-Based Covid-19 Vaccine Candidates [published online ahead of print, 2020 Oct 14]. N Engl J Med. 2020;NEJMoa2027906. doi:10.1056/NEJMoa2027906
[2] Yuan P, Ai P, Liu Y, Ai Z, Wang Y, Cao W, Xia X, Zheng JC. Safety, Tolerability, and Immunogenicity of COVID-19 Vaccines: A Systematic Review and Meta-Analysis. medRxiv [Preprint]. 2020 Nov 4:2020.11.03.20224998. doi: 10.1101/2020.11.03.20224998. PMID: 33173896; PMCID: PMC7654888.
“The views, opinions and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your personal health matters. If you think you are having a heart attack, stroke or another emergency, please call 911 immediately.”



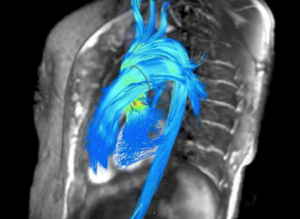
 Figure 1: 3-D CT-FFR coronary tree showing both flow limiting and non-flow limiting lesions [from reference 1].
Figure 1: 3-D CT-FFR coronary tree showing both flow limiting and non-flow limiting lesions [from reference 1].