Heart-Healthy Diet for Women
March is both Women’s History month and National Nutrition month. It’s a good time of the year to pay attention to women’s health in a more constructive way. Heart disease is the #1 cause of death in women, according to a 2017 CDC report1. One in 4 women in the United States dies of heart disease, while only 1 in 30 dies of breast cancer. Within 6 years of having a heart attack, about 46 percent of women become disabled with heart failure. Astonishingly, two-thirds of women failed to make a full recovery after a heart attack2. The risks of heart disease and heart attack increase dramatically after a woman reaches menopause. One in 8 women between 45-64 years old suffers some form of heart disease and the number jumps to one in 4 for women are over 65 years old. Therefore, it’s pertinent to tackle this long-ignored problem, especially for women.

Good progress has been made and continued to be making. The American Heart Association (AHA) launched a movement in 2004, Go Red for Women®, which has reached great success in increasing awareness for heart health in women. Through their relentless efforts in education, innovation, health equity, research development, women are more engaged in preventing and fighting heart disease in the recent decades. Clinical research on cardiovascular disease starts to identify sex difference effects on drug response to help physicians develop a more targeted treatment for women3,4.
To have a healthy heart, besides avoiding some known risk factors such as smoking, drinking and obesity, dietary intervention is one of the most attenable, yet effective ways to live a healthy life. AHA made several educational infographics to promote healthy eating habits. For instance, the figure on the right gives simple suggestions on how to increase diversity of your food choice. It emphasizes the importance of fruits and vegetable consumptions. There are more infographics in the AHA website, if you are interested in learning more, please check it out. Many healthy eating suggestions are developed to combat cardiometabolic diseases. In general, fruits, vegetables, whole grain products, fish, poultry, beans, seeds, and nuts are good for your health, while too many calories, processed food, too much salt/sodium, added sugar, trans-fat and saturated fat are bad for you.
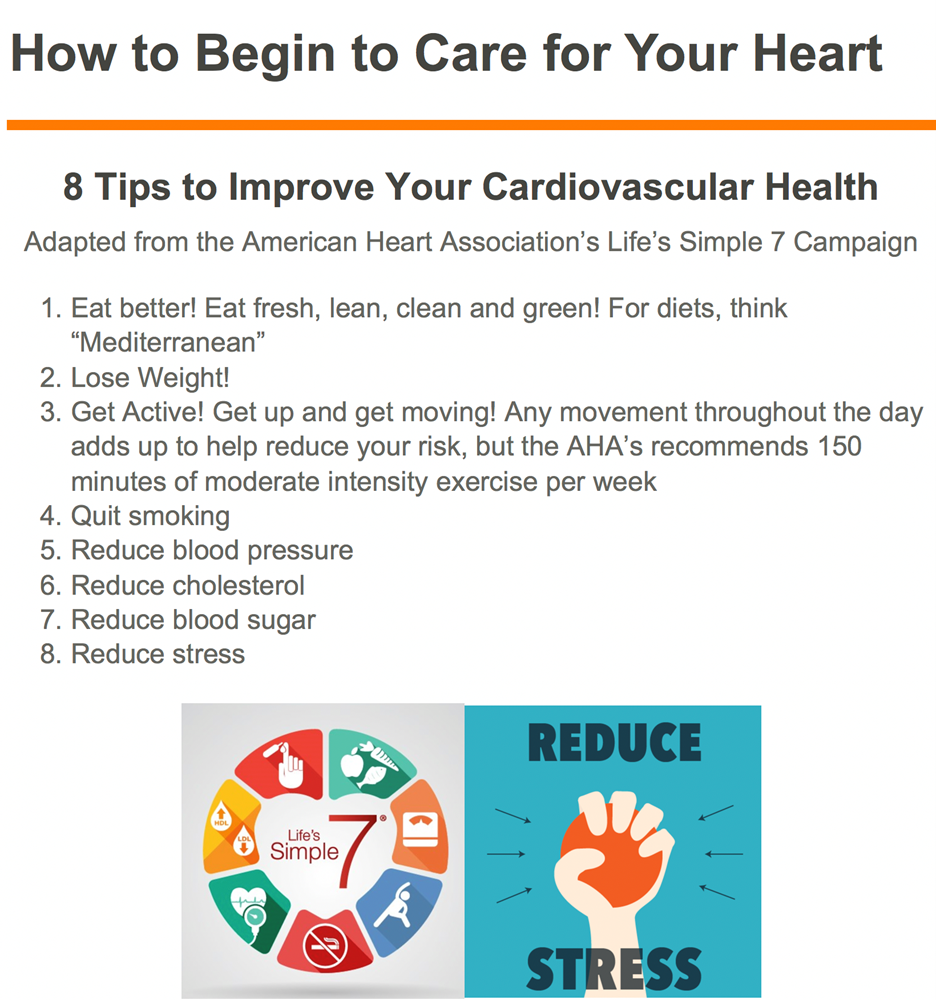
Research shows that Mediterranean diet can reduce risks of cardiovascular diseases5. Table 1 on the right represents a breakdown of Mediterranean diet5. Most of recommended foods are considered general healthy foods. Another study suggests that Mediterranean diet decreases incidences and mortality from coronary heart diseases and stroke in women6.
How to decide which healthy dietary pattern you want follow? Eating index was developed to help evaluate healthy eating habits. Four major indexes including Healthy Eating Index-2015, Alternate Mediterranean Diet Score (AMED), Healthful Plant-Based Diet Index (HPDI), and Alternate Healthy Eating Index (AHEI) all show reduced incidences of cardiovascular disease with healthy eating patterns7. If you have trouble deciding which eating habit you want to develop, just follow the general recommendation first. After all, a little bit of deviation won’t change the overall benefits. The key is to stick to it and keep consistent.
References
- Heron M. Deaths: Leading Causes for 2017. National vital statistics reports : from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System. 2019.
- Sandmaier Marian A4 – National Heart, Lung, and Blood Institute MA-S. The healthy heart handbook for women. 2005:1 online resource (106 pages) : illustrations (some color)-Other US.
- Jin X, Chandramouli C, Allocco B, Gong E, Lam CSP, Yan LL. Women’s participation in cardiovascular clinical trials from 2010 to 2017. Circulation. 2020.
- Scott PE, Unger EF, Jenkins MR, Southworth MR, McDowell TY, Geller RJ, Elahi M, Temple RJ, Woodcock J. Participation of Women in Clinical Trials Supporting FDA Approval of Cardiovascular Drugs. Journal of the American College of Cardiology. 2018.
- Anon. Primary prevention of cardiovascular disease with a mediterranean diet. Zeitschrift fur Gefassmedizin. 2013.
- Fung TT, Rexrode KM, Mantzoros CS, Manson JE, Willett WC, Hu FB. Mediterranean diet and incidence of and mortality from coronary heart disease and stroke in women. Circulation. 2009.
- Shan Z, Li Y, Baden MY, Bhupathiraju SN, Wang DD, Sun Q, Rexrode KM, Rimm EB, Qi L, Willett WC, Manson JAE, Qi Q, Hu FB. Association between healthy eating patterns and risk of cardiovascular disease. JAMA Internal Medicine. 2020.
“The views, opinions and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your personal health matters. If you think you are having a heart attack, stroke or another emergency, please call 911 immediately.”