New Guidelines on the Most Effective, Most Accessible Health Intervention on the Planet Released at #AHA18
The new physical activity guidelines from DHHS were released, not coincidentally I suppose, on “Sneaker Day” at #AHA18. I walked up the 5th floor of McCormick place to hear Adm. Brett Giroir, MD, Assistant Secretary for Health present the update. I was excited to see this one, because I’m a lover of activity— running, yoga, strength training, dance, martial arts, hiking, swimming, etc. Activity makes me feel good, and I’ve seen the change in other people (friends, patients) who’ve become active. And because, as a clinician who works with underserved people, I love health promotion activities that are free.
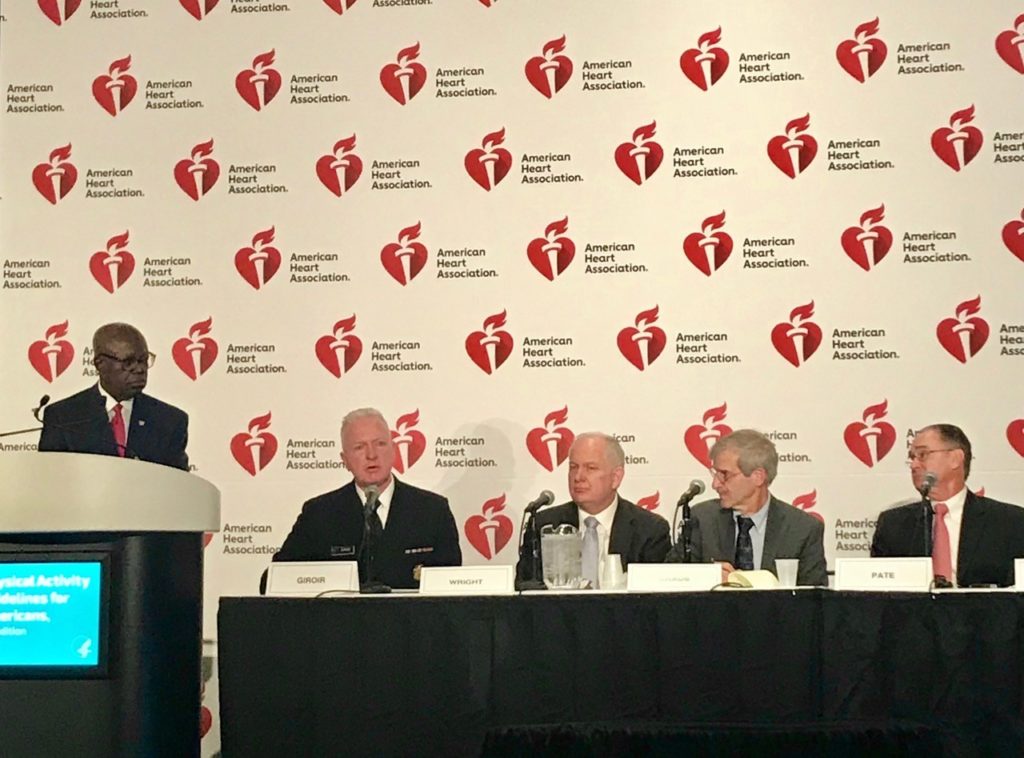
I was curious to hear what the approach would be. Much of the “big news” at AHA is related to drug and intervention trials. Physical activity is a different kind of topic— one that isn’t necessarily the primary domain of many of the attendees. How would this group from HHS fit in? Giroir said, “Our overarching goal is to transform the current sick-care system into a health-promoting system.” Here, here! Not only is this intuitively appealing, but it better aligns with value-based payment systems that are coming down from on high. We’ve heard a lot about trying to align financial incentives in less perverse ways, so let’s keep a watchful eye on that. I like interventions that are free— but there’s a big machine out there that doesn’t agree, and it can be hard to get the same kind of traction.
So that said, what’s in the new guidelines? There aren’t big shifts in the actual recommendations, but there’s an important change in the messaging.
- First, the guidelines address the need for activity in all people, including toddlers (for the first time), people with chronic illnesses, pregnant and post-partum women, and older adults. Message: activity matters for everybody.
- The next key point is that all activity counts— it doesn’t need to be in designated sessions and it doesn’t matter if it’s just a few minutes at a time. The target numbers haven’t changed– but the message now includes that people should “move more and sit less” throughout the day, and any activity is better than none. As physical therapist Dr. Kelly Starrett says, the best position is the next position. This messaging also suggests that not only is activity healthful, but sedentary time is detrimental to health. It’s a two-sided coin, and it’s important to think of it that way. We’ve heard “sitting is the new smoking”– and the evidence here suggests that’s not off the mark. The key message is that activity that’s part of the day-to-day way we live is important to our health. I’ve said this a lot to patients, but it’s great to have the guidelines– and evidence– back it up. The recommendation to get activity throughout the day should strengthen support for programs that encourage movement in all kinds of contexts.
- The last major theme is that activity is even better for us than we previously knew. Much of the evidence reviewed isn’t about what to do, or how, or even how much— but rather, that any and all activity is healthy in ways we hadn’t previously described and measured. Health benefits are immediate, and include lower anxiety, lower blood pressure, better sleep, and better insulin sensitivity. Long-term benefits include reduced cancer risks (including types for which the benefits were previously not described), better brain health, less weight gain, and fewer risky falls. For those with chronic illnesses, it can reduce pain, symptoms, and disease progression and improve cognition. It’s a testament to our physical activity research community (including lots of great work presented this week!) that we have all this data. Can we turn this data into action? We can’t do it exclusively in a clinical setting, despite our best intentions. We’ll need implementation studies. We’ll need CBPR. We’ll need policy advocacy.

Just 26% of men and 19% of women meet the current guidelines. The bar in these guidelines isn’t high. This tells me that we need to work on systems. Schools, workplaces, and public spaces are low-hanging fruit. Chapter 8 of the guidelines also touches on faith-based settings and mass media campaigns. Dan Buettner’s The Blue Zones is an example of a program that’s ahead of the curve, working with communities to tweak infrastructures and build social communities to keep activity in the fabric of life. Michelle Obama’s “Let’s Move” project took a stab at the public messaging approach. What else could we try? In a Viewpoint article for JAMA, Giroir & Wright make some systems suggestions, and also touch on the potential for wearable tech and workplace initiatives to move the needle. These are well-trodden paths, and we’re still waiting for strong evidence of efficacy. Personally, I’d like to see rules and norms encourage activity-friendly clothing and footwear in professional  settings (#SneakerDay every day!?). Can we make it “OK” to stand for a bit when our tracking devices remind us that we’ve been sitting for an hour? Can we support activity with locker rooms at work? Better and more accessible training for healthcare workers on exercise prescription? More clarity on the roles and qualifications of fitness professionals? #AHA18 had a heart failure “Hackathon” this year to generate novel ideas– can we come up with some innovative ways to improve implementation of the cheapest, most effective treatment we have for poor health?
settings (#SneakerDay every day!?). Can we make it “OK” to stand for a bit when our tracking devices remind us that we’ve been sitting for an hour? Can we support activity with locker rooms at work? Better and more accessible training for healthcare workers on exercise prescription? More clarity on the roles and qualifications of fitness professionals? #AHA18 had a heart failure “Hackathon” this year to generate novel ideas– can we come up with some innovative ways to improve implementation of the cheapest, most effective treatment we have for poor health?
References:
U.S. Department of Health and Human Services. Physical Activity Guidelines for Americans, 2nd Edition. Washington, DC: U.S. Department of Health and Human Services; 2018.
Giroir BP & Wright D. (2018). Physical activity guidelines for health and prosperity in the United States. JAMA, published online 11/12/18.