The American Heart Association (AHA) Stroke Council, one of the 16 councils within the AHA, is one of the largest councils within the organization. Amongst the awards it bestows at the major stroke-related conferences worldwide is the Stroke Council Award, a prestigious prize awarded to a single investigator at the AHA Scientific Sessions annually.1 Selection is made from amongst ‘those who actively work to integrate stroke and heart disease in clinical care, education or research’.1
This year, the award went to Dr. Bruce Ovbiagele, MD, MSc, MAS, MBA, MLS, FAAN, FAHA, who is a Professor of Neurology and an Associate Dean at the University of California, San Francisco.2 Dr. Ovbiagele has worked on stroke care for the underserved both in the US and in Sub-Saharan Africa and has >500 publications, >100,000 citations, and an h-index of >80.3 He has previously served as a member of the NIH-NINDS Advisory Council, Chair of the International Stroke Conference, Officer of the World Federation of Neurology, and is currently a part of of the FDA Peripheral & Central Nervous System Drugs Advisory Committee.2
Dr. Ovbiagele’s award lecture at the AHA (Session Number ST.AOS.380), titled ‘Different Strokes for Different Folks: Achieving a Higher Health Equity Say-Do Ratio’ focussed on the disparities in stroke burden and outcomes for different populations (Figure 1). Citing data from the AHA 2020 Update on Heart Disease and Stroke Statistics, Dr. Ovbiagele highlighted how African-Americans continue to have the highest stroke incidence and mortality rate of all communities, with African American men aged 45-54, for instance, having three times the mortality rate than their white counterparts.4 Dr. Ovbiagele stressed upon the widely reported and consistently poorer outcomes for women after stroke, coupled with the increased disability and lower quality of life.5 These disparities may have been further exacerbated by women having a lower likelihood of receiving thrombolysis.5,6,7
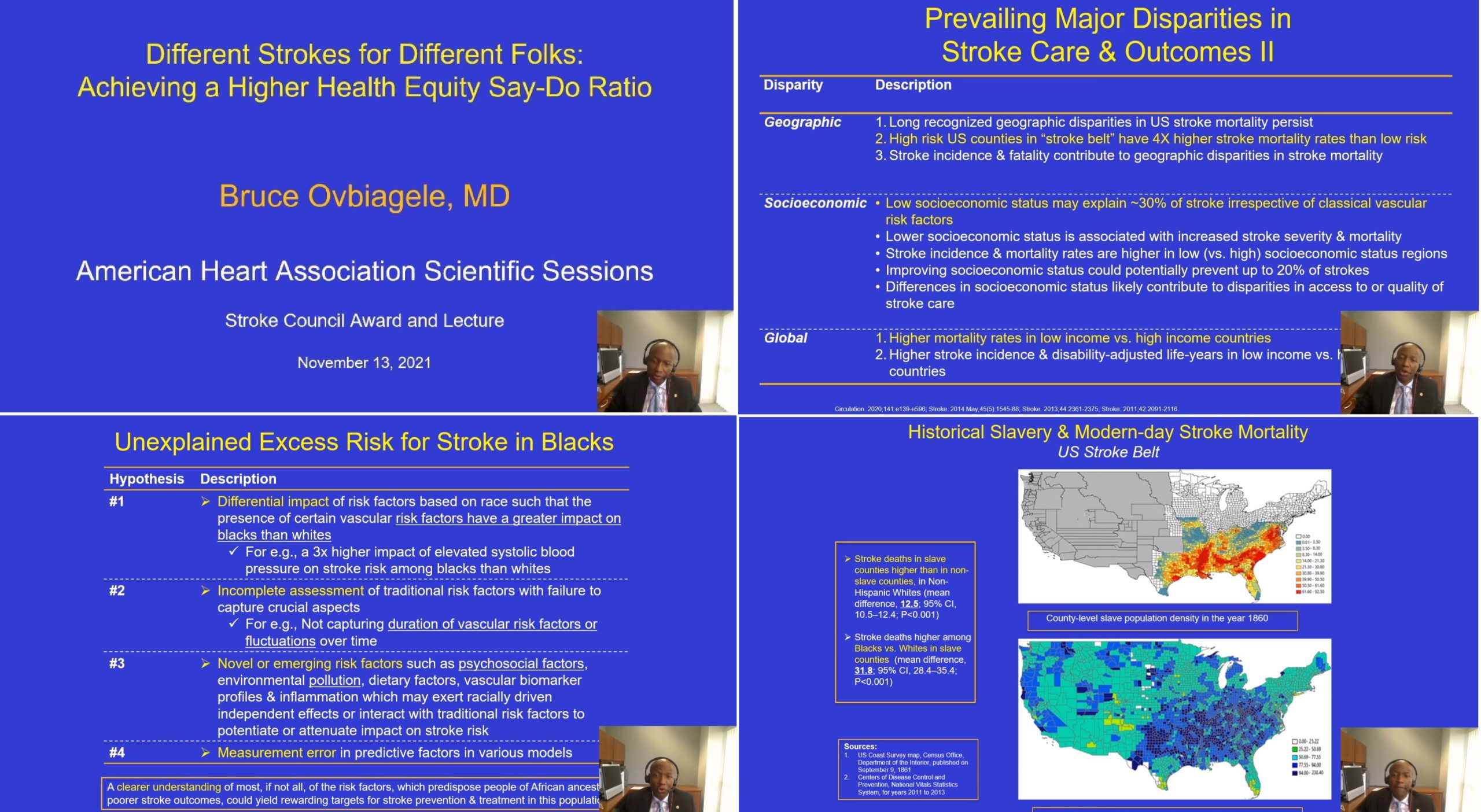
Figure 1
More than a decade ago, the AHA/ASA had put out a policy statement describing in clear terms how minority populations continue to receive suboptimal treatment for both primary and secondary stroke prevention strategies in comparison to whites.7 Health equity in stroke, however, seems to be a long way from home, with little progress reflected in the AHA 2021 Stroke Statistics Update, when put beside the AHA 2011 Update. Poorer outcomes for stroke continue to be pervasive globally, but even in high-income countries, the disparities between populations remain substantial. These disparities are evident at all levels, from stroke prevalence, first stroke incidence, stroke recurrence, to mortality.7,10
Summarizing the prevailing hypotheses (effect modification or differential impact, measurement errors, incomplete assessment, novel emerging factors) on why African Americans have an unexplained higher risk of stroke despite adjustment, Dr. Ovbiagele noted that a better comprehension of these risk factors could produce valuable opportunities for stroke prevention. Dr. Ovbiagele added a greater nuance for the audience that for different racial and/or ethnic minorities, indicators of socioeconomic status are not equivalent. In addition, they have higher exposure to multiple psychosocial stressors, which in turn have been demonstrated to increase stroke risk. For instance, Egido et al’s data from INTERSTROKE demonstrated a 30% and 35% increase in stroke risk by psychosocial stress and depression, respectively.11 Dr. Ovbiagele then raised the yet unclear question of the existence of racial differences in the susceptibility and/or resilience to these psychosocial factors.
Dr. Ovbiagele laid down the various perspectives around the arguments of race being not a biological construct, but a social construct. These perspectives are well-reflected in the 2020 pledge by the board of directors of the American Medical Association (AMA) on ending racial essentialism.12 Willarda Edwards, MD, the Chair of the AMA Task Force on Health Equity, captured this elegantly as: “Recognize that when the race is described as a risk factor, it is more likely to be a proxy for influences including structural racism than a proxy for genetics”.12
References:
- American Heart Association. Stroke Council Award and Lecture. Available at: https://professional.heart.org/en/partners/awards-and-lectures/lectures/stroke-council-award-and-lecture Accessed Nov 14, 2021
- American Academy of Neurology. Boards of Directors. Available at: https://www.aan.com/about-the-aan/board-of-directors-bruce-ovbiagele/ Accessed Nov 14, 2021
- Google Scholar Profile. Bruce Ovbiagele. Available at: https://scholar.google.com/citations?user=dqwMdcYAAAAJ&hl=en Accessed Nov 14, 2021
- Virani SS, Alonso A, Benjamin EJ, et al. Heart Disease and Stroke Statistics-2020 Update: A Report From the American Heart Association. Circulation. 2020;141(9):e139-e596. doi:10.1161/CIR.0000000000000757
- Bushnell C, McCullough LD, Awad IA, et al. Guidelines for the prevention of stroke in women: a statement for healthcare professionals from the American Heart Association/American Stroke Association [published correction appears in Stroke. 2014 Oct;45(10);e214] [published correction appears in Stroke.2014 May;45(5):e95]. Stroke. 2014;45(5):1545-1588. doi:10.1161/01.str.0000442009.06663.48
- Virani SS, Alonso A, Benjamin EJ, et al. Heart Disease and Stroke Statistics-2020 Update: A Report From the American Heart Association. Circulation. 2020;141(9):e139-e596. doi:10.1161/CIR.0000000000000757
- Cruz-Flores S, Rabinstein A, Biller J, et al. Racial-ethnic disparities in stroke care: the American experience: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42(7):2091-2116. doi:10.1161/STR.0b013e3182213e24
- Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics–2011 update: a report from the American Heart Association [published correction appears in Circulation. 2011 Feb 15;123(6):e240] [published correction appears in Circulation. 2011 Oct 18;124(16):e426]. Circulation. 2011;123(4):e18-e209. doi:10.1161/CIR.0b013e3182009701
- Virani SS, Alonso A, Aparicio HJ, et al. Heart Disease and Stroke Statistics-2021 Update: A Report From the American Heart Association. Circulation. 2021;143(8):e254-e743. doi:10.1161/CIR.0000000000000950
- Howard VJ, Kleindorfer DO, Judd SE, et al. Disparities in stroke incidence contributing to disparities in stroke mortality. Ann Neurol. 2011;69(4):619-627. doi:10.1002/ana.22385
- AMA: Racism is a threat to public health. American Medical Association. Published Nov 16, 2020. Available at: https://www.ama-assn.org/delivering-care/health-equity/ama-racism-threat-public-health Accessed Nov 14, 2021
- Egido JA, Castillo O, Roig B, et al. Is psycho-physical stress a risk factor for stroke? A case-control study. J Neurol Neurosurg Psychiatry. 2012;83(11):1104-1110. doi:10.1136/jnnp-2012-302420
“The views, opinions and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your personal health matters. If you think you are having a heart attack, stroke or another emergency, please call 911 immediately.”