The 2022 American College of Cardiology (ACC) meeting was held in Washington DC. It was the first ACC meeting offering both in-person and virtual participation. After two years of uncertainty about the future of scientific meetings, hopefully, the COVID-19 pandemic was under control, and the cardiovascular community had the opportunity to meet colleagues, friends, and mentors/mentees once again. A day before the conference, the 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure was released. A year ago, the 2021 Expert Decision Pathway for heart failure Treatment Optimization was released; however, the emerging new therapies available for heart failure necessitate the early update of heart failure (HF) guideline.
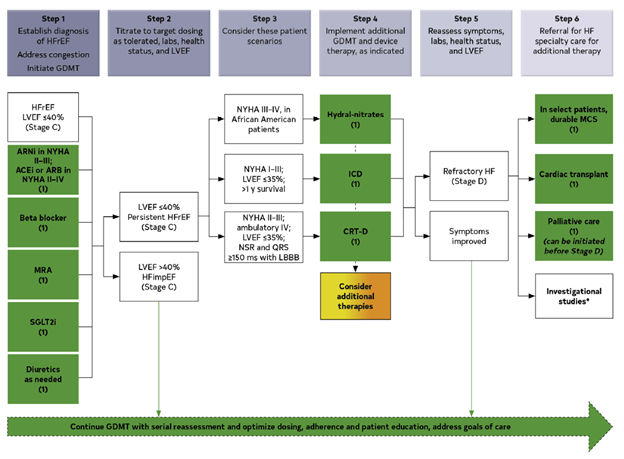
Guideline directed medical therapy (GDMT) for heart failure with reduced ejection fraction (HFrEF: LVEF EF≤ 40%) and heart failure with mildly reduced ejection fraction (HFmrEF: LVEF 41%–49%) now includes four-pillar medications: sodium-glucose cotransporter 2 inhibitor (SGLT-2i), angiotensin receptor neprilysin inhibitor (ARNI)/ angiotensin-converting enzyme inhibitor (ACEi)/angiotensin receptor blocker (ARB), beta-blockers and mineralocorticoid receptor antagonist (MRA). New recommendations for patients with heart failure with preserved ejection fraction (HFpEF: LVEF ≥ 50%) were made for the first time. SGLT2i (Class of Recommendation 2a), MRAs (Class of Recommendation 2b), ARNIs (Class of Recommendation 2b), and ARB (Class of Recommendation 2b) are now the cornerstone of HF therapies in patients with HFpEF. Avoidance of routine use of nitrates or phosphodiesterase-5 inhibitors (Class of Recommendation 3: No Benefit) was endorsed in this patient population. Health care professionals also need to understand drugs that may worsen HF. In patients with HFrEF, non-dihydropyridine calcium channel-blocking, class IC antiarrhythmic medications and dronedarone, thiazolidinediones, dipeptidyl peptidase-4 (DPP-4) inhibitors (Saxagliptin and Alogliptin) and Non-steroidal anti-inflammatory drugs should be avoided (Class of Recommendation 3: Harm). In patients with HFrEF without a specific indication, such as atrial fibrillation, or venous thromboembolism, anticoagulation is not indicated (Class of Recommendation 3: No Benefit).
The new guideline also revised the definition for HF stages. Stage A (At risk for HF) was defined as patients with hypertension, cardiovascular disease, diabetes mellitus, obesity, exposure to cardiotoxic agents, or a family history of cardiomyopathy. Stage B (Pre-HF) was defined as patients without current or previous HF symptoms/signs but evidence of structural heart disease, increased filling pressures or elevated stress cardiac biomarker (persistent elevated cardiac troponin or natriuretic peptide). Stage C: patients with current or previous symptoms/signs of HF, and stage D (advanced HF): patients with marked HF symptoms that interfere with daily activity with recurrent hospitalization despite optimized GDMT. The guideline provides therapies for patients at each stage of HF to prevent the progression of HF.
Moreover, the 2022 HF guideline endorsed five additional therapies once GDMT has been optimized. Ivabradine (Class of Recommendation 2a) was recommended for patients with HFrEF, New York Heart Association (NYHA) I-III, in normal sinus rhythm, heart rate ≥70 beats per minute on a maximally tolerated beta-blocker. Vericiguat (Class of Recommendation 2a) for patients with LVEF <45%. Digoxin (Class of Recommendation 2b) for symptomatic HFrEF. Polyunsaturated fatty acids (Class of Recommendation 2b) for HF NYHA II-IV and potassium binders (Class of Recommendation 2b) for patients with HF with hyperkalemia while taking renin-angiotensin-aldosterone system inhibitors. Further recommendations were provided for select patients with HF and anemia, iron deficiency, hypertension, atrial fibrillation, malignancy, sleep disorder, and mitral regurgitation. I would highly recommend my blog readers to review this enlightening just-released HF guideline: https://www.ahajournals.org/doi/10.1161/CIR.0000000000001063
“The views, opinions, and positions expressed within this blog are those of the author(s) alone and do not represent those of the American Heart Association. The accuracy, completeness, and validity of any statements made within this article are not guaranteed. We accept no liability for any errors, omissions, or representations. The copyright of this content belongs to the author and any liability with regards to infringement of intellectual property rights remains with them. The Early Career Voice blog is not intended to provide medical advice or treatment. Only your healthcare provider can provide that. The American Heart Association recommends that you consult your healthcare provider regarding your health matters. If you think you are having a heart attack, stroke, or another emergency, please call 911 immediately.”